What is a peptic ulcer?
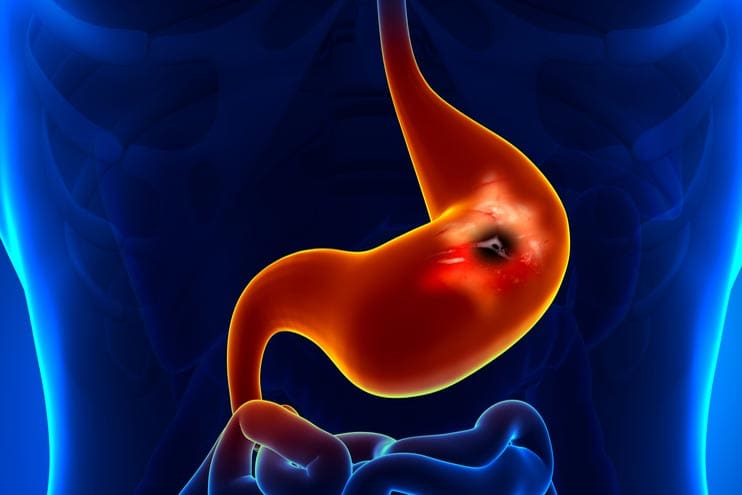
A peptic ulcer is a lesion or sore on the protective lining of the stomach (where it is called a gastric ulcer) or duodenum. Doctors often define it as a mucosal break greater than 3-5 mm in the stomach or duodenum, with a visible depth.
Peptic ulcers are a common condition – they used to affect men more than women, but now their occurrence is similar in men and women.
Symptoms
Peptic ulcers do not always cause signs or symptoms, but some of the symptoms of peptic ulcer are:
- Upper abdominal pain. The usual symptom of an ulcer is pain in the upper part of the abdomen just below the breast bone. It is often a burning or ‘knife-like’ pain which goes through to the back. The pain generally occurs when the stomach is empty (a few hours after meals) and will often wake the sufferer at 2 or 3 o’clock in the morning. The pain is often relieved by food or antacid medication.
- Heartburn may occur, although this is more often a symptom of gastro-oesophageal reflux
- Indigestion.
- Nausea (feeling sick).
- Loss of appetite.
- Unexplained weightloss.
- Anaemia may occur due to blood loss, which may happen slowly. Symptoms of anaemia include tiredness, shortness of breath with exercise, and pale skin colour.
- Vomiting blood. This is a more serious symptom that happens if the ulcer bleeds.
- Passing blood in the bowel motions. Also a serious symptom as a result of the ulcer bleeding. If this happens the motions have a black, ‘tar-like’ appearance.
- Perforation. On rare occasions an ulcer will perforate (form a hole) through the stomach or duodenal wall. This is a major emergency requiring surgery and may be life-threatening.
Risk factors for peptic ulcer
Ulcers are areas of damage to the lining of the stomach (gastric ulcer), or the upper part of the intestine (duodenal ulcer).
The 2 most common risk factors for peptic ulcer are Helicobacter pylori (a bacterium that lives in the stomach), and long term use of NSAIDs (non-steroidal anti-inflammatory drugs).
Helicobacter pylori
Many people with ulcers have an infection in the stomach with a bacterium known as Helicobacter pylori. H. pylori infection is particularly important in the development of duodenal ulcers. The bacteria cause ongoing inflammation of the stomach lining.
It is estimated that up to 4 of every 10 adults in the world are infected with Helicobacter pylori, but not every one of them will go on to develop an ulcer. Thirty per cent of Australians are estimated to be infected, but infection rates are greater for Indigenous Australian communities. It’s not clear why some people with H. pylori seem to be resistant to developing ulcers.
H. pylori is more common in older age groups. It is often acquired in childhood and the increased incidence in older people may reflect living conditions in earlier years, more than it does age.
NSAIDs
Long-term use of NSAIDs (non-steroidal anti-inflammatory drugs), such as aspirin, ibuprofen and naproxen, is linked to an increased risk of peptic ulcer. This is because most NSAIDs are associated with an increased risk of damage to the gastrointestinal mucosa.
Other factors
Other factors which additionally may increase the risk for peptic ulcers, and make them more difficult to treat, include smoking, alcohol and stress.

Tests and diagnosis
Your GP may refer you to a gastroenterologist for tests and treatments, depending on your symptoms, age and medical history.
Peptic ulcers can be diagnosed by endoscopy, where a flexible telescopic tube is passed through your mouth down into the stomach and duodenum, allowing the doctor to examine the tissues. If they find an ulcer, they may take a small sample (biopsy) to test for H. pylori bacteria.
The doctor will probably also want to test you for H. pylori – usually by a breath test. H. pylori can also be tested for by a blood test or a stool test.
Treatment
Your doctor will probably suggest you take H. pylori eradication therapy. Eradication of H. pylori greatly reduces the likelihood of ulcers recurring and the need for long-term acid suppression therapy. Most ulcers respond well to this therapy.
Eradication of H. pylori takes the form of triple therapy – a proton pump inhibitor (esomeprazole) and the 2 antibiotics amoxicillin and clarithromycin – taken for a week. Examples of brand names of triple therapy are Esomeprazole Sandoz Hp7 and Nexium Hp7.
The proton-pump inhibitor suppresses acid production in the stomach and allows healing to take place.
There are alternative medicines for people allergic to penicillin.
Triple therapy will heal most active peptic ulcers and eradicate H. pylori in 70-80 per cent of cases. Some more complicated ulcers will also need a short maintenance course of a proton-pump inhibitor until the ulcer is confirmed to be healed.
People with NSAID-induced ulcers should ideally stop taking the NSAIDs (on their doctor’s advice). If this is not possible, they may need to take a proton-pump inhibitor also for a prolonged time to suppress excess acid production in the stomach.
People whose ulcers are linked to H. pylori should also stop taking NSAIDs if they can. But always check with your doctor.
Very rarely, peptic ulcers cause complications, and surgery is necessary to stop bleeding.
What should you do if you have ulcer symptoms?
If you have symptoms suggestive of a peptic ulcer, see the doctor.
This common condition is easily managed and serious complications are usually preventable.