What is cirrhosis of the liver?
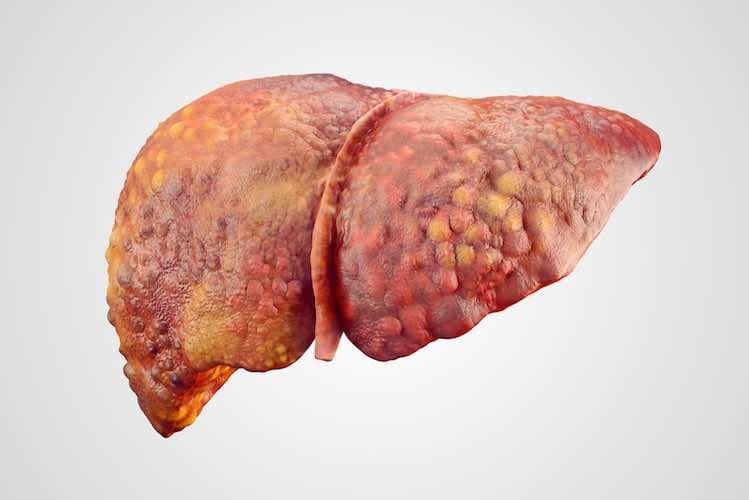
Cirrhosis is a type of severe and irreversible liver disease caused by long-term liver damage. Healthy liver tissue is progressively replaced by scar tissue in a process called fibrosis. The scar tissue damages the normal structure of the liver, which in turn affects the flow of blood through the liver. Without proper blood flow, the liver can’t carry out its normal functions. As scar tissue builds up, the liver itself becomes distorted, hard and lumpy. Cirrhosis increases the risk of developing liver cancer, which is the most rapidly rising cause of death from cancer in Australia.
Why is a healthy liver important?
The liver is the body’s largest organ and is essential to keep the body functioning properly. The liver carries out many important tasks, including:
- Producing bile to break down fats;
- ‘Detoxifying’ the body by removing toxins or harmful chemicals;
- Breaking down alcohol;
- Producing cholesterol and proteins, which are essential for many of the body’s functions;
- Storing vitamins; and
- Controlling clotting of the blood after an injury.
With the liver so heavily involved in many important processes, it’s easy to see how an unhealthy liver – like one affected by cirrhosis – can affect the functioning of the entire body.
What causes cirrhosis?
Cirrhosis happens when there is long-term damage to the liver over a long period. The liver becomes inflamed in an attempt to heal the damage. This repeated cycle of inflammation and healing results in severe scarring of the liver. Cirrhosis of the liver can be caused by a variety of factors, including:
- Long-term heavy drinking of alcohol – It usually takes about 10 years of heavy alcohol consumption for cirrhosis to develop. However, women can develop cirrhosis with a daily intake of 2-3 alcoholic drinks a day, which might not be considered by some people to be ‘heavy’. Similarly, men who have 3-4 alcoholic drinks a day can also eventually develop cirrhosis;
- Chronic viral hepatitis types B, C and D – Several different types of viruses can cause inflammation of the liver. If not treated, the liver becomes progressively more damaged and this can result in cirrhosis after several decades;
- Non-alcoholic fatty liver disease – In this condition, fat accumulates in the liver, which causes inflammation and cirrhosis. This disorder is becoming increasingly common due to the high level of fat in our diets and the increase in conditions such as obesity, high blood pressure, high cholesterol and diabetes;
- Haemochromatosis – This is one of the most common inherited disorders in Australia. Too much iron is absorbed by the body and the excess is deposited in the liver and other organs;
- Wilson’s disease – This is a rare inherited disorder where excessive amounts of copper are absorbed in body tissues, particularly the liver;
- Other inherited metabolic disorders – Certain disorders (such as cystic fibrosis) interfere with the body’s metabolism and change the way the liver stores particular substances. These disorders can result in cirrhosis;
- Autoimmune hepatitis – This condition is due to a problem with the body’s immune system. The immune system mistakenly recognises its own liver cells as ‘foreign’ and produces antibodies that attack the liver, resulting in inflammation;
- Blocked bile ducts – Bile is made in the liver and the bile ducts carry the bile out of the liver to the gallbladder where it is stored. If the bile ducts become blocked due to scarring or inflammation, bile backs up in the liver and damages the liver tissues, which can lead to cirrhosis. Primary biliary cirrhosis is a disease of adults where the bile ducts become damaged. Biliary atresia affects babies that are born without bile ducts, or the bile ducts are damaged, causing a build-up of bile in the liver;
- Toxic hepatitis – This is rare and is caused by severe reactions to medicines (such as paracetamol overdose), toxins or chemicals;
- Chronic congestive heart failure with liver congestion – Repeated episodes of congestive heart failure with liver congestion can cause cirrhosis of the liver; or
- Cirrhosis of unknown origin – In about 10% of cases, no cause for cirrhosis is found. This type of cirrhosis is called cryptogenic cirrhosis.
What are the initial symptoms of cirrhosis?
In the early stages of liver disease, there may be no symptoms at all, or only minor, non-specific changes such as:
- Loss of appetite;
- Weight loss;
- Tiredness and weakness; or
- Nausea (feeling sick).
Later symptoms and problems
As cirrhosis progresses and liver function decreases, other symptoms can develop, including:
- Ascites – This is a build-up of fluid in the abdominal cavity. It occurs because the damaged liver cells can’t make as much protein as normal, which leads to fluid being retained in the body. Increased blood pressure in the veins taking blood from the intestines also causes fluid to leak into the abdominal cavity. In addition, fluid can build up in the legs (especially the lower legs), where it is known as oedema;
- Bruising and bleeding – You may bruise more easily because the liver can no longer produce enough proteins that are needed to clot the blood after an injury;
- Intense itching – This is due to bile products being deposited in the skin;
- Jaundice – The scarring of the liver causes an increase in blood levels of a coloured pigment called bilirubin that is normally secreted by liver cells. This leads to yellowish discolouration of the skin and the white part of the eyes;
- Spider naevi – These are enlarged or swollen blood vessels in the skin with a spidery appearance. They can often be seen on the face and chest of people with cirrhosis;
- Gallstones – These small gritty deposits can occur in cirrhosis because not enough bile is being secreted from the liver, so not enough bile reaches the gallbladder;
- Reddening of the palms of the hands;
- Enlarged breast tissue in men – This occurs because the damaged liver cells can no longer break down the hormone oestrogen properly, so levels build up and lead to swelling of the breast tissues (doctors call this gynaecomastia);
- Psychological changes – A liver damaged by scarring can’t effectively filter toxins. A build-up of toxins in the blood – particularly ammonia – can cause psychological changes (this is called hepatic encephalopathy). At first, the changes may be mild, such as poor concentration, forgetfulness, confusion or not being able to complete simple tasks. But as cirrhosis progresses, they may progress to significant personality changes or even falling into a coma;
- Sensitivity to medicines – Most medicines taken by mouth are absorbed from the digestive tract into the bloodstream. They then pass through the liver. When the liver is damaged by cirrhosis, it does not filter medicines as effectively. This can lead to the build-up of medicines in the body, which may increase side effects from medicines;
- Swollen blood vessels – Veins in the oesophagus (food pipe) can become swollen due to an increase in pressure in the vein that supplies blood to the liver. The scarring of liver tissue makes it harder for blood to flow through the liver, so the blood pressure increases. Blood backs up in surrounding small veins that line the stomach and oesophagus and they become swollen. These small veins are fragile and can burst if the pressure becomes too great, which can lead to internal bleeding. Bleeding into the stomach may cause vomiting of blood, while bleeding into the intestines may result in dark, tar-like bowel movements (faeces).
How is cirrhosis diagnosed?
It’s important to diagnose liver disease (including cirrhosis) as early as possible. By the time major symptoms appear, there has already been significant damage to the liver and the condition becomes harder to treat.
Your doctor can usually diagnose cirrhosis by:
- Asking about your symptoms and how they have developed;
- Doing a physical examination – Your doctor can feel whether your liver is enlarged by gently pushing on your belly.
If your doctor thinks it might be cirrhosis, other tests might be requested, including:
- Blood tests to check how well your liver is working;
- Scans of your liver – such as a CT scan, MRI scan or regular ultrasound scan – to ‘look’ at the size, shape and structure of the liver;
- A special ultrasound scan called Fibroscan (see below) that measures liver stiffness;
- An endoscopy where a long, thin flexible tube is passed down your oesophagus (food pipe) into your stomach to check for swollen blood vessels; or
- A liver biopsy – A fine needle is inserted between the ribs to remove a small sample of liver cells to check for damage.
What is a Fibroscan?
A Fibroscan is a special type of ultrasound that is can check the ‘hardness’ or stiffness (also called fibrosis) of your liver. As the liver becomes progressively more damaged, the liver tissue becomes stiffer. The scan is painless and doesn’t involve needles or invasive instruments, and only takes 10-15 minutes. A probe is placed on your lower chest, above the liver. The probe sends out a vibration wave (a pulse) that bounces off the liver. The reflected wave can tell your doctor how stiff your liver is. The stiffer your liver, the more likely that your liver has fibrosis or cirrhosis. Your liver is given a score, which is usually interpreted in the context of what sort of liver disease you have:
- 2.5 – 7.4 suggests minimal fibrosis (stiffness);
- 7.5 – 9.4 suggests moderate fibrosis; and
- 9.5 or higher suggests severe fibrosis or cirrhosis.
Fibroscan is increasingly being used to diagnose cirrhosis as a painless alternative to a liver biopsy. The scan can also be used to track the progression of liver damage over time. Fibroscan results are also important when determining the most appropriate treatment for hepatitis C.
How is cirrhosis treated?
There is no cure for cirrhosis. The condition can be fatal if liver damage is severe, but it generally takes years to reach this stage. Cirrhosis is irreversible, so the treatment aims to stop the disease from getting any worse. The treatment you are offered will depend partly on the cause of your cirrhosis:
- Cirrhosis due to too much alcohol – If you are a heavy drinker, you will need to stop consuming alcohol. Your doctor will be able to provide you with a comprehensive plan to help you quit drinking. The outlook for your disease is not good if you continue to drink, whereas the benefits of stopping are enormous. You will halt the progression of the disease from day one and will also feel much better. Talk to your doctor today. There are many methods available to help you;
- Cirrhosis due to viral hepatitis – You may be treated with anti-viral drugs to reduce permanent damage. Treatment of hepatitis B and C in the early stages is increasingly successful at preventing cirrhosis. New treatments for hepatitis C have recently become available in Australia that are more effective and easier to take compared to previous medicines;
- Cirrhosis due to fatty liver disease – Weight loss and taking medicines to control other conditions (such as diabetes and high blood pressure or cholesterol) are useful;
- Cirrhosis due to haemochromatosis – Venesection, the drawing of blood, is the treatment to prevent further damage.
- Autoimmune hepatitis – Medicines that decrease inflammation (such as corticosteroids) or damp down the immune system (such as immunosuppressants) may be prescribed; or
- Cirrhosis due to Wilson’s disease – This is treated with medicines to remove excess copper from the body. Similarly, cirrhosis caused by haemochromatosis is treated by the regular removal of a quantity of blood to get rid of excess iron from the body.
Some symptoms of cirrhosis can be helped by taking medicines, having a medical procedure, or making lifestyle changes:
- Medicines known as diuretics can help remove excess fluid in people who are retaining too much fluid;
- A low-sodium diet and restricting fluid intake can also help reduce fluid build-up;
- A medicine called lactulose syrup and a low-protein diet can help reduce the psychological symptoms of cirrhosis, such as confusion and forgetfulness. High-protein meals increase levels of toxins in people with liver damage;
- Blood pressure-lowering medicines can help reduce blood pressure in the veins supplying the liver;
- Swollen blood vessels in the oesophagus (food pipe) may be able to be treated by a variety of procedures through an endoscope (a thin flexible tube passed down into the oesophagus and stomach);
- Creams or ointments can help stop or reduce any itching; and
- A healthy balanced diet, maintaining a healthy weight and avoiding alcohol are essential for everyone with cirrhosis.
Is there a link between cirrhosis and liver cancer?
Having cirrhosis of the liver increases the risk of developing a type of liver cancer (called hepatocellular carcinoma). Liver cancer is often fatal, although surgery and chemotherapy medicines can prolong life for several years.
When is a liver transplant necessary?
If cirrhosis is severe and the liver stops working, liver transplantation is the only option. It is often recommended when symptoms become difficult to control by other methods. Liver transplantation may also be necessary if someone with cirrhosis develops liver cancer, and surgery or chemotherapy are not an option or not successful. Liver transplants are not usually given to people with cirrhosis who are actively using alcohol or drugs. However, people who have cirrhosis as a result of heavy drinking who can show that they have stopped may still be good candidates for transplantation.