Diverticular disease is a condition in which small pockets or out-pouchings called diverticula occur in the wall of the bowel. Diverticula can remain trouble-free or they can become inflamed or infected and cause symptoms, which is known as diverticulitis. Diverticulitis can be a medical emergency.
What’s the difference between diverticulitis and diverticulosis?
- Diverticulitis is when the out-pouchings become inflamed or infected.
- Diverticulosis is when the out-pouchings are present without any inflammation.

What causes diverticulitis?
Eating a low-fibre (‘Western’) diet results in stools with a hard consistency that require high pressures to be generated in the bowel in order to push stools along and pass them. Diverticular disease is thought to result from these high pressures in the bowel forcing the lining of the bowel to pocket outwards through the surrounding muscle layer of the bowel, causing pouches.
Diverticulitis occurs when faecal matter becomes lodged in the pouches and causes inflammation or infection.
Risk factors
Diverticular disease is common, especially in countries like Australia where people generally eat a low-fibre diet. A third of Australian adults aged over 45 have it and about half of Australians older than 75 years, although for most their diverticula cause them no problems and they don’t know they have it. People who eat a diet high in fibre are much less likely to develop diverticular disease.
Young people who are obese have a raised risk, and more women than men have diverticular disease.
Symptoms of diverticulosis
Diverticular disease generally causes no symptoms – only 1 in 4 people with it will have symptoms. Some people have:
- Alternating bowel habit that alternates between constipation and diarrhoea.
- Intermittent lower abdominal pain, usually on the left side, brought on by eating and that’s relieved by passing wind or going to the toilet.
- Bloating.
Diverticulitis symptoms
A mild attack of diverticulitis may come and go of its own accord in a few days. However, diverticulitis can be a medical emergency. If the pouches retain faeces they can become inflamed and infected causing signs and symptoms of diverticulitis that may include:
- Left-sided abdominal pain: The most common symptom of diverticulitis is left-sided abdominal pain that doesn’t go away. It may persist for several days. Asian people may experience pain on the right-hand side.
- Tender abdomen: especially on the lower left side.
- Mild cramping.
- Fever or high temperature.
- Bloating.
- Constipation or diarrhoea
- Nausea, feeling sick and/or vomiting.
- Loss of appetite.
- Change in bowel habit.
- Rectal bleeding: bright red blood passed from the rectum.
Some of these symptoms are common to many conditions, so their presence does not always mean you have diverticular disease, but you should see your doctor as soon as possible for advice if they occur. Some people with diverticulitis will go on to develop complications.
Complications
If complications develop, symptoms can include bleeding from the bowel (when a blood vessel in the pouch breaks), or increasing and persistent pain and fever (when an abscess develops and/or ruptures or the pouch itself ruptures into the abdominal cavity). Although rare, these complications of diverticulitis are serious and usually require emergency treatment in hospital.
The most common serious complications of diverticulitis are:
- Sudden and significant bleeding from the bowel. This is usually bright red blood and painless, but requires admission to hospital. Many cases stop bleeding spontaneously, but a blood transfusion is sometimes necessary.
- Abscess: This is a collection of pus that forms in the infected pouch. Antibiotics may clear up the abscess, or it may need to be drained surgically.
- Perforated bowel: This is when a hole develops in the infected pouch in the bowel wall.
- Peritonitis: If the perforation in the bowel wall leaks pus into the abdominal cavity, it will cause peritonitis. Peritonitis can be fatal and needs immediate attention. Fortunately, peritonitis from diverticulitis is rare.
- Fistulas: A fistula is an abnormal connection or channel that forms between 2 organs of the body or an organ and the outside of the body. Diverticulitis may cause fistulas between the bowel and the bladder, or the bowel and the vagina. They arise in diverticulitis if infection causes the organs to stick together. Fistulas may need surgical repair.
- Bowel obstruction: this is when the bowel (colon) becomes blocked either partially or completely. It is caused by scarring from the infection. If the bowel is totally blocked emergency surgery will be necessary.
Diagnosis
Diverticulosis, when the pouches are not inflamed or infected, is often diagnosed by chance during investigations for other bowel problems.
These may include:
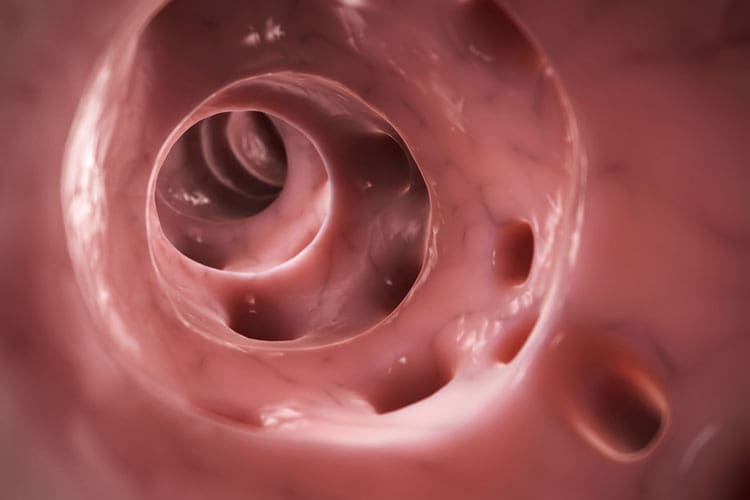
- Colonoscopy: a thin tube with a lighted camera is inserted into your rectum and the doctor can see the pouches, if there are any.
- Barium enema: pouches can be easily seen on a barium enema test, although this test is rarely done now.
Diverticulitis is usually diagnosed during investigation for an attack that’s in progress. To diagnose diverticulitis your doctor will first discuss your medical history and your symptoms and do a physical examination. They may suggest you first have tests to exclude other diseases as the cause of your symptoms.
Some of the tests and examinations that may be done are:
- Pelvic examination: Women may need a pelvic examination to rule out any problems in the pelvis.
- Digital rectal examination: The doctor inserts a gloved finger into your rectum to check for any tenderness or blockage.
- Blood test: This may be done to check your white cell count, to see if there are any signs of infection and to check your red cell count, to see if you are losing blood somehow.
- CT scan of the abdomen: a CT scan is a type of X-ray – this can show up inflamed pouches of the bowel and confirm a diagnosis of diverticulitis. This is usually the definitive investigation to confirm diverticulitis.
Colonoscopy and barium enema are not usually done when a person is having an attack of diverticulitis because of the risk of perforating the bowel or spreading infection.
Treatment of diverticulosis
People with bowel pouches which have not become inflamed are generally recommended to:
- Change to a high-fibre diet (see below) to reduce the risk of symptoms and complications developing.
- Consume plenty of fluids (to avoid constipation).
- Take bulk-forming laxatives, if they cannot achieve a high-fibre diet otherwise, or they get constipation or diarrhoea. Examples are unprocessed wheat bran or psyllium seed husks (available from pharmacies under various brand names).
Treatment of diverticulitis
When the bowel pouches have become inflamed (diverticulitis), treatment is aimed at:
- Resting the bowel, initially with a low-residue diet (low fibre or fluid-only).
- Relieving pain with analgesic medicines (painkillers), usually paracetamol. Don’t take aspirin or ibuprofen as they increase the risk of internal bleeding and stomach upsets.
If there are signs of a generalised infection, such as a raised white cell count or fever, then also:
- Fighting infection with antibiotics.
Treatment of a mild attack of diverticulitis may be carried out at home, and if caught early enough may respond to antibiotics in a few days.
If there are serious complications of diverticulitis, such as significant bleeding, an abscess that isn’t healed with antibiotics, rupture of pouches, or pain that can’t be managed, then hospital treatment will be required, which may include transfusion to replace lost blood, stronger painkillers (than paracetamol) and intravenous fluids, given by a drip. A small number of people will require emergency surgery to remove the affected area of bowel. This may result in them having a temporary colostomy.
Sometimes non-emergency surgery is planned to remove an area of bowel containing diverticula which have caused recurring diverticulitis in the past or which have joined onto another structure such as the bladder.
Keyhole (laparoscopic) surgery can sometimes be carried out for non-urgent removal of diseased areas.
Prevention
There are some lifestyle changes you can make that will reduce the likelihood of you getting diverticular disease and that will lessen the chance of an attack of diverticulitis.
- An adequate intake of dietary fibre keeps stools soft and prevents constipation. Good sources of dietary fibre are apples and pears, along with other fresh fruits, vegetables and wholegrain cereals. Baked beans and legumes, such as kidney beans and lima beans, are very high in fibre, but may cause problems with wind in some people. A simple way to increase the fibre in your diet is to add a bulking agent such as unprocessed wheat bran or psyllium seed husks. Australian recommendations for fibre intake are 30 g fibre/day for men and 25 g fibre/day for women.
- Regular exercise protects against developing it.
- Adequate water intake will help process the fibre and keep stools soft.
What to eat if you have diverticular disease
Sometimes people are given advice to avoid certain foods, such as nuts, pips, seeds and corn, however, there is no real evidence to support this advice. As mentioned above, ensure you have a good fibre intake and drink enough water to keep your stools soft.
Does diverticular disease cause cancer?
There doesn’t seem to be any link between diverticular disease and bowel cancer. Having diverticulosis or diverticulitis does not increase the risk of getting bowel cancer.
Remember …
- Most people don’t have any symptoms.
- People who develop diverticulitis in most cases get better quickly with antibiotic treatment.
- Complications of diverticulitis that require surgery are serious, but occur in only a minority of people.
- The most important aspect of managing diverticular disease and avoiding both symptoms and complications is eating a diet that is high in fibre.