Is Silicosis curable? With thousands of workers potentially exposed to dangerous silica particles while working with engineered stone, it’s a question weighing heavily on the mind of many Australians. Associate Professor Jane Bourke from the Biomedicine Discovery Institute at Monash University and her team, including researcher Dr Paris Papagianis, are working to better understand silicosis. “Historically, silicosis caused by sandblasting, tunneling, quarrying and mining dates back to the 1900s,” they explain. “The number of silicosis cases in the Australian community is due to the increasing use of engineered stone in home renovations over the last 20 years. We know that the risk of silicosis is particularly high with this product due to its high silica content and unsafe work practices that have exposed workers to dangerous levels of dust.” Here, Associate Professor Bourke and Dr Papagianis share their insights, advice on testing, early diagnosis and what hope there is for a cure of this devastating lung disease.
What is silicosis?
Silicosis is an occupational lung disease affecting stonemasons, miners and tunnellers. When these workers cut, crush, drill or polish materials that contain silica, such as engineered stone bench tops or natural sandstone, this generates crystalline silica dust particles that are so small, they lodge deep in the lungs and cause inflammation and irreversible scarring in the lungs.
What are the symptoms of silicosis?
The most common symptoms are shortness of breath, difficulty breathing and persistent cough. Depending on disease severity, individuals may also feel fatigued or weak.
What should I do if I’m worried about having silicosis?
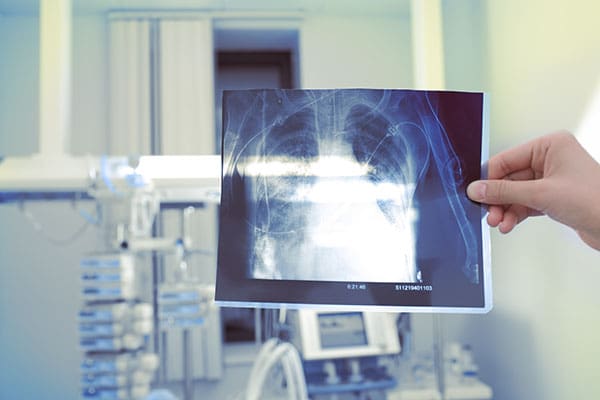
You can ask your local GP or lung doctor for testing if you are working as or have worked as a stonemason, particularly if you have worked with engineered stone containing high silica content. The lung doctor may ask you to perform a questionnaire about your level of potential exposure, lung function tests and an X-ray or High Resolution CT (HRCT) scan of your lungs.
Who is at most at risk of developing silicosis?
Workers who are exposed to high amounts of inhalable silica dust over prolonged periods are at risk of silicosis. The highest risk occupations are in workplaces such as engineered stone manufacturing, tunnelling, quarrying, mining, construction, ceramics, brick making or paving/surfacing. There are approximately 600,000 Australian workers currently exposed to silica dust, including about 4400 stonemasons.
If silicosis is associated with engineered stone bench tops, is there any risk if you have one in your home?
No. Engineered stone is not dangerous when it is in its solid form and already installed in the home. Engineered stone is only dangerous when it is being cut, polished or crushed as this produces the dust particles that can be breathed into the lungs. Special care should be taken when it is being removed during a renovation to avoid generation of silica dust.
Is silicosis like asbestosis?
In some ways silicosis is like asbestosis. Both are caused by inhalation of harmful particles and the symptoms are also similar, with scarring of the lungs leading to breathing difficulties. However, unlike asbestosis, silicosis can develop in just two to five years after exposure to dust, whereas asbestos typically develops over decades.
Does silica exposure cause mesothelioma like asbestosis?
No. Silicosis increases the risk of developing lung cancer but does not cause mesothelioma, which is a rare and aggressive type of cancer that affects the cell layer around many organs including the lung.
How many Australians are experiencing silicosis?
The first reported case of engineered stone-induced silicosis in Australia was in 2015. As of February 2023, we know that more than 600 workers across Queensland, New South Wales and Victoria have silicosis, but this is likely an underestimate of the actual case numbers in the community. Based on the total number of Australian workers already exposed, it is expected that more than 100,000 people will have silicosis. Of these, more than 10,000 will develop lung cancer.
How can Australia eradicate silicosis?
While we know that silicosis is incurable, it is preventable. Banning engineered stone, made up of 95 per cent silica, would reduce worker exposure in that one industry, and alternative safer materials could be used for kitchen bench tops. However, stonemasonry is not the only high-risk occupation for developing silicosis. Silica is also found in sand, stone, concrete and mortar, so it is critical that workers in quarries, mines and tunnels are also protected from the dust generated from these other materials and have their health monitored regularly.
How is silicosis diagnosed? Who should ask for testing?
It is important that anyone currently or previously working in a high-risk industry with silica dust exposure has regular checks of their lung health. Some workplaces will be monitoring their employees, but it’s important that workers also let their GP know their occupational history, even if they have no symptoms.
Diagnosis is based on three main steps:
1) a survey to work out the likely level of silica dust exposure
2) a lung function test at a hospital
3) an X-ray or HRCT scan of the lungs
If you have been exposed to silica dust, have reduced lung function for your age and have signs of scarring or injury on your lung X-ray, you may be diagnosed with silicosis.
A GP or a lung specialist can request these tests but they can only be conducted by specialised occupational or respiratory physicians. A list of specialists can be found at The Royal Australasian College of Physicians website.
Why is early detection of silicosis important?
Unfortunately, there is no cure for silicosis. Detection of early signs of disease is critical, as it might then be possible to remove yourself from environments with harmful levels of silica dust. Preventing further exposure is the only way to reduce the risk of more lung damage.
How is silicosis treated?
The treatment of silicosis is based on a person’s medical history and stage of disease. As with any lung diseases, cessation of smoking and vaping is essential, as well as vaccinations to avoid lung infections that might make symptoms worse. An ongoing management plan with your respiratory physician is necessary as – for example – oxygen might be needed. Because the lungs are not able to get rid of the silica dust already inhaled, the only way to treat silicosis, as a last resort, is with a lung transplant .
How long can people live with silicosis?
Each person diagnosed with silicosis experiences the disease differently. This is likely due to a variety of factors, including general heath, history of smoking and level of exposure. Some people with silicosis show a rapid decline in lung function, which restricts their day-to-day activities and can cause early death. Some will develop other diseases, such as lung cancer, as a consequence of silicosis. Others with mild disease can remain stable with few symptoms and continue to work and maintain a good quality of life over many years.