What is haemophilia?
Haemophilia is an inherited bleeding disorder where blood doesn’t clot properly. It is caused when blood does not have enough clotting factor. A clotting factor is a protein in blood that controls bleeding.
There are two types of haemophilia. Both have the same symptoms:
- Haemophilia A is the most common form and is caused by having reduced levels of clotting factor VIII (8).
- Haemophilia B, also known as Christmas Disease, is caused by having reduced levels of clotting factor IX (9).
Haemophilia is not contagious.
There is also another bleeding disorder known as acquired haemophilia, which is not inherited like the classical form of haemophilia. This is a very rare condition where a person’s immune system develops antibodies against one of their body’s own clotting factors and results in a reduced factor level in their blood. Acquired haemophilia usually develops when people are older and can affect both men and women.
How common is haemophilia?
Haemophilia is rare. In Australia there are more than 2,800 people with haemophilia, who are nearly all male. Approximately one in 6,000 males has haemophilia A. Haemophilia B is less common and approximately one in 25,000-30,000 males has it. Haemophilia is found in all races and all socio-economic groups. Haemophilia in females does occur but is very rare. However, some females who carry the genetic alteration that causes haemophilia can also have bleeding problems.
What happens when you have haemophilia?
Haemophilia is a lifelong condition. It can’t be cured, but with current clotting factor treatments it can be managed effectively.
The common belief that people with haemophilia could bleed to death from a cut is a myth. A person with haemophilia does not bleed any faster than anyone else, but the bleeding continues for longer if it is not treated and may lead to a delay in healing. Minor cuts and scratches are not a problem and need only 2 3 a Band-Aid® and some pressure at the site of bleeding. With deeper cuts or injuries, bleeding continues for longer if blood does not form a tough, adherent clot where the blood vessels have been damaged. Specialised treatment will then be needed so blood can clot normally.
Internal bleeding episodes or ‘bleeds’ are the main problem for most people with haemophilia. Bleeds are most commonly into joints or muscles. They can happen without an obvious cause (sometimes called ‘spontaneous’), or as a result of injury.
If internal bleeding is not stopped quickly with treatment, it will result in pain and swelling. Over a period of time, repeated bleeding into joints and muscles can cause permanent damage, such as arthritis in the joints, and chronic pain.
Bleeds into the head, spine, neck, throat, chest, stomach or abdominal area are much less common but can be life-threatening. If this happens, the person with haemophilia should attend an emergency centre immediately and the Haemophilia Centre should also be contacted.
There is at least one specialist Haemophilia Centre in every Australian state or territory, located in a major public hospital. The Haemophilia Centre has a team of health professionals, including doctors, nurses, physiotherapists, and social workers or counsellors, who specialise in the treatment and care of people with bleeding disorders.
Levels of severity
There are three levels of severity in haemophilia: mild, moderate and severe. The level of severity depends on the amount of clotting factor in the person’s blood. A person with haemophilia will have the same level of severity over their lifetime, eg a person with severe haemophilia will always have severe haemophilia. Within a family, males with haemophilia will also have the same level of severity, eg if a grandfather has severe haemophilia and his grandson has inherited haemophilia, his grandson will also have severe haemophilia.
The normal range of factor VIII and factor IX in a person’s blood is between 50% and 150%.
Levels of severity of haemophilia
Mild haemophilia 5-40% of normal clotting factor
- Usually only have bleeding problems after having teeth taken out, surgery or a bad injury or accident.
- Might never have a bleeding problem.
Moderate haemophilia 1 – 5% of normal clotting factor
- Might have bleeding problems after having teeth taken out, surgery or a bad injury or accident
- May have bleeding problems after minor injuries, such as sporting injuries
- Rarely have a bleed for no obvious reason.
Severe haemophilia Less than 1% of normal clotting factor
- Often have bleeds into joints, muscles and soft tissues
- Can have bleeds for no obvious reason, as well as after surgery, dental work or injuries including minor bumps or knocks
Signs and symptoms of haemophilia
How is haemophilia diagnosed?
Haemophilia is usually diagnosed through:
- The physical signs that a person has unusual bleeding problems and,
- checking the family history for bleeding problems and,
- laboratory tests on a blood sample for a person’s clotting factor levels. If a male has low factor VIII levels, he has haemophilia A. If he has low factor IX levels, he has haemophilia B. The laboratory tests will show whether he has mild, moderate or severe haemophilia.
First signs of haemophilia
Children with severe haemophilia are usually diagnosed in the first year when their parents or health professionals notice unusual bruising or bleeding problems or there is a family history of haemophilia. Most babies with haemophilia do not have bleeding problems at birth. However, some bleeding problems may appear at birth or soon after. Haemophilia may be suspected if babies have internal bleeding or unusual swelling or bruising after delivery, continue to bleed after a heel prick or after circumcision, or have excessive bruising after immunisation.
If there is a family history of haemophilia, a sample of the baby’s blood can be tested after birth to check the factor VIII or IX levels and see whether the baby has haemophilia. Testing should be repeated when the baby is six months of age to confirm the results. Testing can also be done during pregnancy to determine if the baby has haemophilia.
When all babies begin to crawl and walk, they can knock into hard objects as well as having twists, falls or sitting down with a bump. Small bruises are common in children with severe haemophilia and are not usually dangerous or painful – the padding of “baby fat” is a natural protection. Bruising easily might be the first sign they have a bleeding problem. As with anyone, a knock or bang or bruise on the head needs some extra attention. In a child with severe haemophilia, these might become serious and should be checked by a haemophilia specialist. Sometimes toddlers or children may have a bleed into a joint. Painful swelling or reluctance to use an arm or a leg can be a sign that a bleed has taken place. The specialist nurses and physiotherapists at the Haemophilia Centre can advise on haemophilia issues during these normal childhood stages.
Children with haemophilia can have all the normal immunisations at the usual age. Informing the nurse or doctor giving the immunisation that the baby or toddler has haemophilia is important. Injections can be given subcutaneously, into the fatty tissue under the skin, rather than into the muscle, and pressure put on the skin where the child was injected. This reduces the risk of bruising and bleeding. However, changing the way of giving immunisations isn’t necessary for all children with haemophilia. If you have a child with haemophilia, contact the Haemophilia Centre for advice on how your child should be immunised.
As children grow they learn to recognise that bleeding may be occurring. Even before pain or swelling becomes obvious they may recognize a “funny feeling” which is one of the earliest signs of a joint bleed.
Mild or moderate haemophilia might not be diagnosed until children are older, or sometimes until they are adults. If they have mild haemophilia, minor injuries may heal normally because there is enough clotting factor activity in the blood. The bleeding problem might not be noticed until the person has surgery, a tooth taken out or a major accident or injury.
Growing up with haemophilia
With treatment and support from their Haemophilia Centre, most people with haemophilia can live relatively normal healthy lives. Haemophilia treatment has changed a great deal in recent years. Unless there are complications, young people can expect to grow up with fewer or no joint problems from their haemophilia. With sensible precautions, they can play most sports, exercise and look forward to a full and productive life.
Although the level of haemophilia severity usually doesn’t change during a person’s lifetime, people tend to have more bleeding episodes as children than as adults. The reasons for this are not clear. Sometimes also the factor VIII level rises in later adult years in people with mild haemophilia A. This rarely occurs in people with haemophilia B.
Inheritance and haemophilia
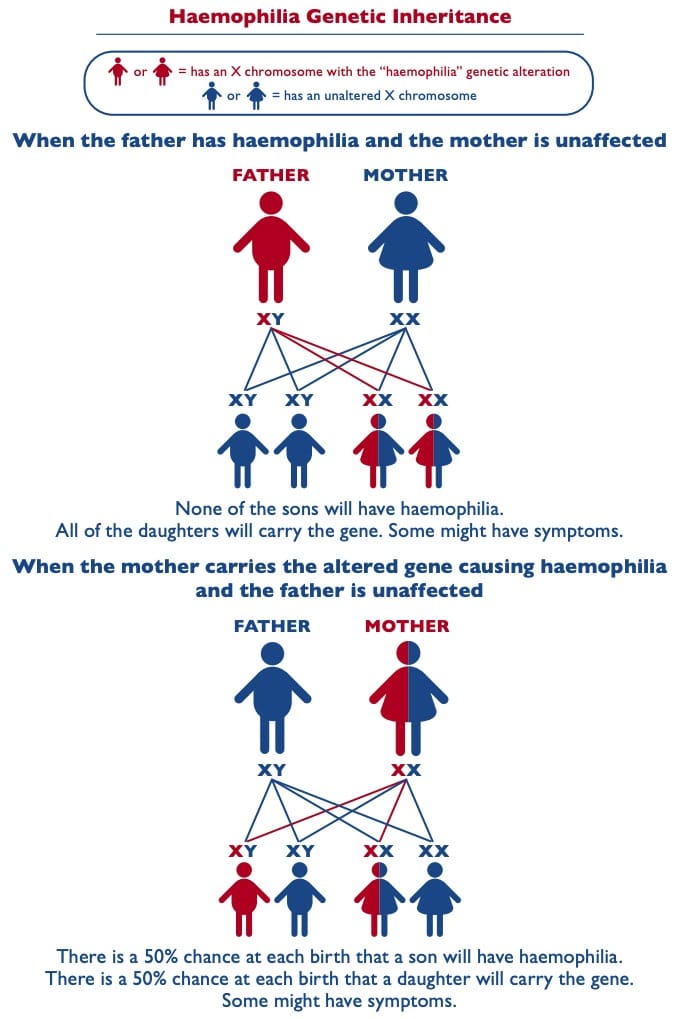
Haemophilia is an inherited condition and occurs in families. Haemophilia is caused by a mutation or alteration in the gene making factor VIII or IX, and this altered gene is commonly called the “haemophilia gene”. This altered gene is passed down from parent to child through generations. Men with haemophilia will pass the altered gene on to their daughters but not their sons. Women who carry the altered gene may pass it on to their sons and daughters. Sons with the altered gene will have haemophilia. Daughters with the altered gene may have normal or reduced factor VIII levels and some will not have symptoms, while others may have a bleeding tendency.
Cells and chromosomes
Every person has millions of cells that make up their body. At the centre of each cell are 46 chromosomes arranged in pairs. The chromosomes contain the person’s genetic information or ‘genes’, which determine the person’s individual characteristics, such as the colour of their hair or their eyes.
Sex determination
Everyone has a pair of ‘sex’ chromosomes, which decide what gender they are. Each parent contributes one of these chromosomes to their children. Females have two X chromosomes, and receive one from each parent. Males have one X chromosome, which they receive from their mother, and one Y chromosome, which they receive from their father. There are four possible combinations of sex chromosomes that children can receive from their parents.-
The diagram below may assist in understanding this.
Inheritance
The genes for making factor VIII and IX are located on the X chromosome. Because females have two copies of these genes, one inherited from each parent, women with an altered factor VIII or IX gene usually have another copy that is not altered. This helps factor VIII and IX to work properly in the blood clotting process and is often enough to control bleeding.
However, the Y chromosome does not have a gene to produce these factors. Males with an altered factor VIII or IX gene on their X chromosome do not have another factor VIII or IX gene to help with blood clotting and will have haemophilia. If a male with haemophilia has children, all his daughters will carry the haemophilia gene because he will pass the altered factor VIII or IX gene on to them on his X chromosome. His sons will not have haemophilia as his ‘normal’ Y chromosome is passed on to them and they receive their X chromosome from their mother.
Women can carry the genetic alteration causing haemophilia even if they don’t have symptoms. A woman who carries the altered gene can pass it on to both her sons and her daughters. With each pregnancy, there is a 50% chance her male baby will have haemophilia or a 50% chance her female baby will carry the altered gene.
No family history of haemophilia
In about one third of people born with haemophilia, there is no history of the disorder in the family. This happens when a genetic mutation in the factor VIII or IX gene occurs for the first time in the family during reproduction and is passed on at conception. It is often called a new or spontaneous mutation. Once haemophilia appears in a family the altered gene is then passed on from parents to children following the usual pattern for haemophilia. Family members should seek genetic counselling and testing if there is someone in the family who has haemophilia.
Carrying the haemophilia gene
Clotting factor levels and symptoms
Many girls or women who carry the altered factor VIII or IX gene causing haemophilia (the “haemophilia gene”) do not have signs or symptoms of a bleeding disorder.
However, some girls or women who carry this gene have a bleeding tendency. They are often described as “symptomatic carriers”. If their factor levels fall in the range for mild haemophilia (5 – 40% of normal clotting factor), they may sometimes also be referred to as having “mild haemophilia”. In very rare cases, some girls or women have particularly low factor levels causing them to have moderate or severe haemophilia.
Examples of having a bleeding tendency may include:
- Bruising easily
- Heavy menstrual bleeding. This may lead to low iron levels or anaemia
- Excessive bleeding after dental surgery or extractions, other surgery and medical procedures, injuries or accidents
- Prolonged bleeding after childbirth
- Females with very low clotting factor levels may also have joint or muscle bleeds.
All females who carry the gene should have testing for their clotting factor levels. Unlike males with haemophilia, where the factor level is the same within the same family, the factor level in females who carry the gene is unpredictable and varies between family members. Women and girls with lower levels should have theirs checked periodically, as their factor levels may change with age, pregnancy and hormonal medications. If their factor level is low, they will need a treatment plan to prevent bleeding problems and manage any situations that occur.
Genetic testing
A normal factor VIII or factor IX level test will not tell women or girls whether they carry the altered gene causing haemophilia. Some women or girls may have normal factor levels, but still carry the gene.
A common time for testing whether a girl or woman carries the gene is when she reaches childbearing age and can understand the process and implications fully and make the decision for herself. Finding out whether she carries the gene is a process which will take time, sometimes many months. This may involve:
- Discussion with a haemophilia specialist and/or genetic counsellor
- Weighing up the pros and cons of genetic testing with advice and support from specialists, counsellors and other experts – for example, the role of genetic testing in understanding her bleeding disorder; its effect on her perception of herself and on her relationships; her personal understanding of what it’s like to have haemophilia; the impact on children and other family members; her personal religious and cultural beliefs; future disclosure obligations and implications for life or income protection insurance; any costs involved; and other issues relevant to her personal situation
- Looking at the family tree to identify other family members who may carry the gene
- Blood tests for other affected family members (eg, a man with haemophilia) to identify the particular genetic mutation causing haemophilia in her family
- Blood tests for the woman to see if she has the same family genetic mutation.
Many people find that undertaking these tests gives them a lot to think about. The Haemophilia Centre can help with information and advice about genetic testing and can provide a referral to a genetic counsellor, if needed. Women, their partner, parents or family can talk to the Haemophilia Centre or genetic counsellor individually or together prior to testing and many find it helpful.
If a person starts exploring genetic testing but decides against it, there is no obligation to complete the process.
Planning a family
For people with haemophilia or women who carry the gene, planning a family can raise a number of questions:
- Will their children have haemophilia or carry the gene?
- If so, how will this affect them?
- How can they find out?
- What are the options for planning a family?
- How can a mother who carries the gene plan for a safe pregnancy and delivery?
- Who will help with all of this?
Haemophilia Centres can help with questions about having children.
Often people have a particular view of haemophilia based on their memories of their brother, father or grandfather’s experience. Treatment for haemophilia has improved a great deal over the years and it can be valuable to learn more about how haemophilia is treated now and to speak to other people with haemophilia or parents of children with haemophilia or the Haemophilia Centre to see how things have changed. The Haemophilia Centre can also give a referral to a genetic counselling service that specialises in bleeding disorders.
Pregnancy and childbirth
With good management, women who carry the altered gene causing haemophilia have no more problems with delivering a healthy baby than other mothers. However, it is very important to plan and prepare as much as possible.
This involves:
- Ideally, if planning a pregnancy, discussing this with a haemophilia specialist who may refer to a genetic counsellor
- When the pregnancy is confirmed, contacting the Haemophilia Centre for advice on local obstetric services with experience of haemophilia
- Asking the haemophilia and obstetrics teams to consult with each other to plan for a smooth and safe pregnancy and delivery and care for the newborn
- Checking with the Haemophilia Centre before having any invasive procedures, such as chorionic villus sampling or amniocentesis
- Discussing suitable choices for anaesthesia, especially an epidural, with the Haemophilia Centre and obstetrics teams.
A normal vaginal delivery is usually recommended unless there are obstetric complications.
Identifying the sex of the baby
If a pregnant woman knows she carries the altered gene causing haemophilia, it is advisable to determine the sex of the baby before birth, preferably with a non-invasive test with minimal risk to the foetus, such as ultrasound. A male baby is more likely to be affected by haemophilia than a female. The woman and her partner can choose if they want to be told the sex of the baby or not before delivery even if the haemophilia and obstetric teams are aware. If neither the couple nor the medical staff know the sex of the baby and no other genetic testing of the foetus has been carried out, the pregnancy and birth will be managed as if the baby is a male with haemophilia to ensure the baby is delivered safely.
Testing for haemophilia before birth
For a woman or couples who wish to test for haemophilia before birth, there are two main testing options:
- Prenatal diagnostic testing: a test during the pregnancy to check the sex of the baby. If it is male, further testing can check for the family gene mutation or alteration, which will show if the baby has haemophilia
- IVF with pre-implantation genetic diagnosis (PGD): using IVF technology to test embryos for the family gene alteration, before embryo implantation and pregnancy.
For these options to be available the gene alteration in the family must be known.
A genetic counsellor can explore these reproductive options with the woman or the couple in further detail, along with any implications. There may also be substantial costs involved for these tests and procedures and it may be valuable to clarify this and options for support beforehand.
If a pregnant woman has a history of haemophilia in the family and does not know whether she carries the gene, it is important to let the obstetrics team know so that they can plan a safe delivery of the baby with the haemophilia team.
With appropriate treatment haemophilia can be managed effectively.

