Cardiomyopathy is the term used to describe a range of diseases of the heart muscle. Cardiomyopathy can affect people of all ages, including children. In some people, damage to the heart muscle due to cardiomyopathy can weaken the heart and lead to heart failure and dangerous irregular heart rhythms. Treatment depends on the type of cardiomyopathy, and may involve taking medicines or having surgery. In some people, cardiomyopathy is mild and no treatment is needed.
Symptoms
Symptoms and signs will vary depending on the type of cardiomyopathy you have, how severe it is, and your age. Sometimes there are no symptoms, especially in the early stages of the disease.
Symptoms may start or get worse suddenly or gradually, and can include:
- shortness of breath;
- tiredness;
- feeling light-headed or fainting;
- palpitations (an awareness of your heart beating or pounding in your chest);
- swelling in the legs due to fluid build-up; and
- chest pain.
Children with cardiomyopathy may become breathless or have chest pain when exercising or be unable to keep up with their friends while playing. They may also have:
- a cough;
- abdominal pain;
- nausea; or
- reduced appetite.
In babies, signs of cardiomyopathy may include:
- fast or heavy breathing during feeding;
- feeding that takes a long time;
- sweating during feeding; and
- poor weight gain.
Causes of cardiomyopathy in adults
Cardiomyopathy can be classified as either primary or secondary. Primary cardiomyopathy is inherited, or the cause is unknown. Secondary cardiomyopathy is cardiomyopathy that develops as a result of another condition or risk factor.
Causes of cardiomyopathy in adults include:
- Heavy alcohol use over a long time.
- Viral infections. Most viral infections don’t cause heart problems, but occasionally a viral infection can affect the heart, causing cardiomyopathy.
- Hereditary factors. Some types of cardiomyopathy are inherited and affect several members of the same family.
- Coronary heart disease. As well as causing heart attacks, narrowing of the coronary arteries can cause cardiomyopathy.
- Uncontrolled high blood pressure.
- Certain chronic conditions, including diabetes and thyroid disease.
- Sometimes cardiomyopathy can develop during pregnancy.
- Connective tissue diseases such as rheumatoid arthritis, can be associated with cardiomyopathy.
- Conditions such as haemochromatosis, sarcoidosis and amyloidosis can damage the heart muscle.
- Drug use, including cocaine, amphetamines and anabolic steroids, can increase your risk of cardiomyopathy.
- Nutritional deficiencies. Lack of essential nutrients, such as thiamine, can lead to cardiomyopathy.
- Side effects from some cancer treatments (such as certain chemotherapy drugs and radiation therapy) can also cause some types of cardiomyopathy.
Causes of cardiomyopathy in children
In many cases of cardiomyopathy in children, the cause is unknown. Known causes include viral infections of the heart, some metabolic diseases, congenital (present at birth) muscle disorders and certain inherited disorders.
Types of cardiomyopathy
There are several different types of cardiomyopathy, the most common types being dilated cardiomyopathy and hypertrophic cardiomyopathy.
Dilated cardiomyopathy
In dilated cardiomyopathy, the heart muscles stretch (dilate) and the chambers of the heart enlarge. Dilated cardiomyopathy is the most common form of cardiomyopathy in both adults and children.
The dilated heart may lose the ability to contract properly and pump enough blood for the body’s needs. Irregular heart rhythms (arrhythmias) can also occur.
Although no cause is found in many cases, there are numerous conditions that may result in this form of cardiomyopathy. About one-third of people with dilated cardiomyopathy inherit it.
Hypertrophic cardiomyopathy
In hypertrophic cardiomyopathy, the heart muscle thickens (hypertrophies), sometimes making it more difficult for the heart to fill with blood. Hypertrophic cardiomyopathy is common and can affect children and adults. More than half of all cases of hypertrophic cardiomyopathy are inherited.
As the condition progresses, thickening of the ventricles (lower chambers of the heart) can obstruct the flow of blood out of the heart. This affects the heart’s ability to pump properly. Irregular heart rhythms can also occur. Sometimes this form of cardiomyopathy causes cardiac arrest (sudden malfunctioning and stopping of the heart) in teenagers and young adults, often in otherwise fit athletes who previously had no symptoms.
Restrictive cardiomyopathy
Restrictive cardiomyopathy is uncommon in adults and rarely affects children. The cause is often unknown. The muscles of the ventricles become stiff, but not necessarily thickened, making it harder for them to fill with blood between heartbeats. It can lead to heart failure and problems with heart valves.
Arrhythmogenic right ventricular cardiomyopathy (ARVC)
Arrhythmogenic right ventricular cardiomyopathy is rare, usually affecting teenagers and young adults. In this type of cardiomyopathy, scar tissue or fatty tissue develops in the heart muscle, causing arrhythmias (irregular heartbeat). Dangerous arrhythmias and other symptoms can occur after strenuous exercise. It is thought to be inherited.
Broken heart syndrome
A rare type of cardiomyopathy is takotsubo cardiomyopathy, also sometimes called broken heart syndrome or acute stress cardiomyopathy. This type of cardiomyopathy develops after a stressful event, such as death of a loved one. It’s thought that a surge of stress hormones weaken or ‘stun’ the heart muscle. People with this type of cardiomyopathy usually recover completely within days or weeks.
The symptoms of broken heart syndrome, such as chest pain, may resemble those of a heart attack. It’s important to seek immediate medical attention to rule out heart attack. If you experience chest pain, call 000 in Australia for an ambulance.
Complications of cardiomyopathy
There are several serious complications associated with cardiomyopathy. Some types of cardiomyopathy are more likely to cause complications than others.
Heart failure
Heart failure is a common complication and can happen with all types of cardiomyopathy. Heart failure does not mean a sudden giving up of your heart, but is when your heart is not pumping blood around your body as well as it should. It can lead to symptoms such as swollen legs and ankles, as well as feeling short of breath when lying down.
Arrhythmias and sudden death
Arrhythmias are an abnormal heart rhythm. Some types of arrhythmias are life-threatening, and can result in sudden death. Hypertrophic cardiomyopathy can cause sudden cardiac arrest, often in young people.
Problems with heart valves
Having an enlarged heart can affect some of the heart valves, making them leaky. This allows blood to flow in the wrong direction and increases work for the heart.
Blood clots
In some types of cardiomyopathy, especially dilated cardiomyopathy, blood flows more slowly than usual through the heart. Slow blood flow increases the chances of blood clots forming in the heart chambers. If a blood clot breaks free and circulates in the bloodstream (called an embolus), it can be life-threatening if it travels to the brain or a coronary artery and lodges there.
Diagnosis
To diagnose cardiomyopathy, your doctor will ask about your symptoms and perform a physical examination, including listening to your heart sounds with a stethoscope.
Your doctor may recommend the following tests:
- Electrocardiogram (ECG), a simple test that can measure and record the electrical activity in the heart and detect an irregular heartbeat. This test can also be done while exercising – known as an ECG exercise stress test.
- Chest X-ray, which can show the size of the heart and signs of heart failure, such as fluid in the lungs.
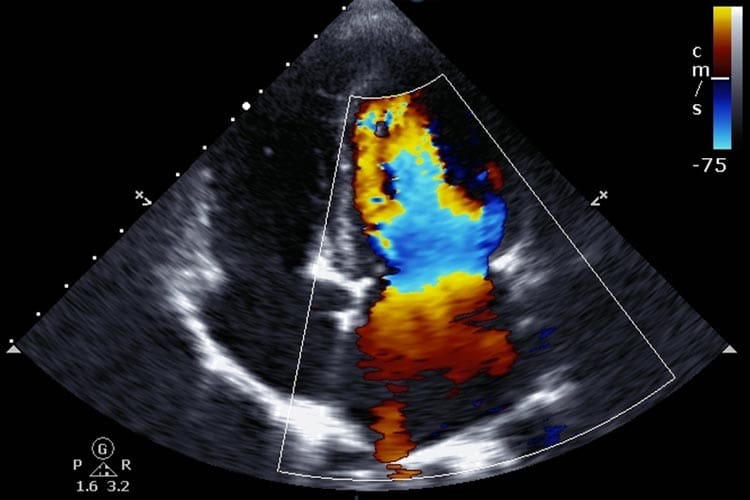
- Echocardiogram (an ultrasound scan of your heart) to show the size of the heart and how it is functioning. It can help to determine the type and severity of the cardiomyopathy. It can also show whether the heart valves are working normally. A stress echocardiogram can show the effect of exercise on the heart.
- In some cases, your doctor may recommend cardiac magnetic resonance imaging (MRI) to confirm the diagnosis or gain more information about your condition.
Other more advanced tests include:
- Cardiac catheterisation, in which a small tube is placed in a blood vessel (usually a vein in your groin) and then threaded up to the heart to measure the pressure inside the heart and blood flow in the heart.
- Myocardial biopsy, in which a small sample (biopsy) of heart muscle tissue is taken for examination under a microscope to help determine the type of cardiomyopathy. The biopsy is taken during cardiac catheterisation.
Genetic tests may also be recommended for some people with cardiomyopathy and their family members, to determine whether they may have an inherited form of cardiomyopathy.
Treatment of cardiomyopathy
If you are diagnosed with cardiomyopathy, your doctor may refer you to a cardiologist (doctor specialising in heart conditions). Children with cardiomyopathy will probably be referred to a paediatrician (doctor specialising in children’s medicine) or paediatric cardiologist.
Treatment for cardiomyopathy is aimed at:
- relieving symptoms;
- preventing further heart muscle damage; and
- treating and preventing complications.
The exact treatment will depend on what sort of cardiomyopathy you have and how severe it is. Some people will not need any treatment. Treatment of secondary cardiomyopathy may involve treating the underlying condition.
Lifestyle measures
Lifestyle choices can do much to help relieve symptoms and improve your quality of life if you have cardiomyopathy. They can also help you avoid complications.
For both adults and children with hypertrophic cardiomyopathy, it’s important to completely avoid strenuous or competitive sports due to the risk of sudden cardiac arrest. Your doctor will be able to advise you on which physical activities are best avoided.
Adults with cardiomyopathy should also:
- quit smoking;
- avoid or cut down on alcohol;
- avoid salty, fatty and highly processed foods;
- maintain a healthy weight;
- reduce stress; and
- get some physical activity (after talking to your doctor about exercise and what is suitable for you).
For the best advice about your particular form of cardiomyopathy, you should talk to your doctor.
Medicines
The medicines used to treat cardiomyopathy depend on the type of cardiomyopathy, your symptoms and risk of complications. They may include:
- anti-arrhythmics to stabilise your heart rhythm;
- anti-hypertensive medicines to control your blood pressure;
- medicines to help improve the ability of the heart to pump effectively and treat heart failure;
- diuretics to help reduce fluid build-up in heart failure; and
- anticoagulants – medicines to help reduce your risk of blood clots.
Surgical procedures
Surgery can help treat certain types of cardiomyopathy, as well as some complications.
For people with hypertrophic cardiomyopathy, removing or destroying some of the thickened heart muscle can improve blood flow out the heart. Septal myectomy is a type of surgery that involves removing some of the thickened heart muscle from the part of the heart called the septum, which separates the heart chambers. In septal ablation, some of the thickened heart muscle is destroyed using an injection of alcohol into the blood vessel supplying that part of the heart.
Heart valve repair or replacement may be recommended for those with leaky heart valves.
People who have an abnormal heart rhythm can have a procedure called radiofrequency ablation, which destroys the area of the heart that the abnormal rhythm is coming from. This is done by inserting a thin tube into a vein your groin and then threading the tube up to your heart. Electrodes on the end of the tube are used to destroy the abnormal area of heart muscle.
Alternatively, a pacemaker can be surgically implanted to control your heart rhythm. An implantable cardioverter-defibrillator (ICD) is sometimes recommended for people who are at risk of a dangerous or life-threatening heart arrhythmia. These implantable devices can detect an abnormal heart rhythm and shock the heart back into a normal rhythm.
For people with severe heart failure as a result of cardiomyopathy a ventricular assist device (VAD), also known as a cardiac assist device (CAD), can be implanted to help your heart pump. These mechanical pumps can be used in people waiting for heart transplants. A heart transplant may be considered if you have severe heart failure and other treatments are not working.
Prevention
In many cases, cardiomyopathy cannot be prevented. However, there are some types of cardiomyopathy that can be avoided, such as those that are caused by excessive alcohol or drug use. Healthy lifestyle choices are important to keep your heart healthy.
If you have several family members who have cardiomyopathy, you may want to ask your doctor about being tested for an inherited form of cardiomyopathy. Finding out that you have inherited cardiomyopathy before you develop symptoms can be lifesaving, especially if you have a type of cardiomyopathy that can cause sudden cardiac arrest. You can adjust your activities and receive treatments to avoid complications.