Your thyroid gland, found at the front of your neck, makes hormones that control your metabolism. There are several conditions that can affect the thyroid, which can mean that it makes too much or too little of these important hormones.
Hypothyroidism (an underactive thyroid) is more common than hyperthyroidism (excess thyroid hormones). Both conditions have a variety of symptoms and causes. Treatments vary according to the type of thyroid condition you have and its severity. In many cases, long-term monitoring and treatment are needed.
Your thyroid gland is in the front of your neck and is divided into 2 lobes (right and left) – one on either side of your windpipe (trachea). The lobes are connected in the middle by a thin bridge of thyroid tissue known as the isthmus. The thyroid gland has been described as being shaped like a butterfly, or a bow tie.

A normal-sized thyroid cannot be seen in the neck and can barely be felt. It’s only when certain conditions result in an enlarged thyroid gland (known as goitre), that a bulge may be seen or felt just underneath the thyroid cartilage (Adam’s apple).
Thyroid hormones
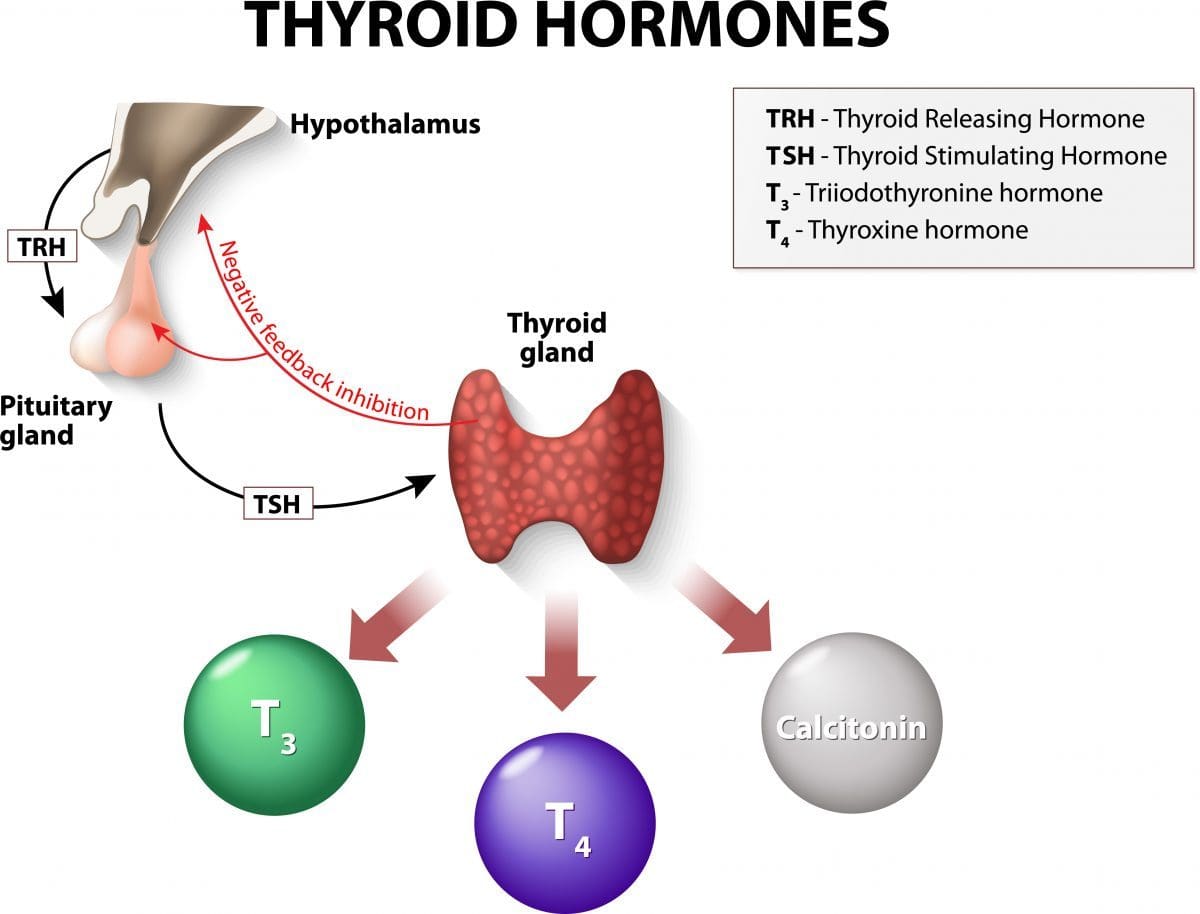
Your thyroid makes 2 main hormones – triiodothyronine (T3) and thyroxine (T4). Adequate amounts of iodine (a chemical element that’s an essential part of our diet) are needed for the thyroid to be able to make these hormones.
Another hormone that’s produced in your thyroid gland is called calcitonin. This hormone, secreted by a small population of cells known as C cells, is involved in regulating the level of calcium and phosphate in your blood.
The main thyroid hormones are secreted directly into the bloodstream and go to all parts of your body. Most T4 is converted to T3 (the active form of the hormone) in your organs and tissues. Thyroid hormones affect your body’s metabolic rate and regulate many of your bodily functions such as breathing, heart rate, body temperature, digestion and how quickly you burn calories.
The amount of hormones your thyroid makes is usually tightly regulated. A part of your brain called the hypothalamus signals your pituitary gland (an important gland in your brain) to produce a hormone called thyroid stimulating hormone (TSH). TSH then signals your thyroid to make T3 and T4. The level of thyroid hormones in your body then feeds back to the hypothalamus and the pituitary, which in turn adjust the release of TSH.
What causes thyroid problems?
Thyroid dysfunction is when too much or not enough thyroid hormones are made. It can be caused by:
- primary thyroid disorders – problems in the thyroid gland itself; or
- central thyroid disorders – problems with the pituitary gland (secondary disorders) or the hypothalamus (tertiary disorders).
While an inadequate intake of iodine is the most common cause of thyroid disease worldwide, autoimmune problems (where your immune system makes antibodies that attack the thyroid gland) are the most common cause of thyroid problems in Australia. Sometimes thyroid problems start during or after pregnancy.
Hyperthyroidism
Hyperthyroidism happens when there is an overproduction of thyroid hormones. It can result in symptoms such as:
- weight loss despite a normal or increased appetite and food intake;
- rapid or irregular heartbeat, which may result in palpitations;
- feeling short of breath;
- often feeling hot or being more sensitive to the heat;
- sweating;
- feeling nervous, anxious or edgy;
- trouble sleeping;
- tremor (shaking), often affecting the hands;
- diarrhoea;
- tiredness;
- muscle weakness; and
- skin and hair changes – thinning of the skin and hair that becomes brittle.
In women, irregular periods is a common symptom.
Causes of hyperthyroidism
Graves’ disease, an autoimmune condition, is the most common cause of hyperthyroidism in Australia. In Grave’s disease, antibodies made by your immune system stimulate your thyroid to make too much thyroxine. It can cause swelling of the thyroid (goitre) and thyroid eye disease. It usually affects people aged between 20 and 60 years of age, and is much more common in women than in men.
Other common causes of hyperthyroidism include the following.
- Toxic thyroid nodule or toxic multinodular goitre – conditions where non-cancerous growth(s) develop in the thyroid and produce excessive amounts of thyroxine.
- Thyroiditis (inflammation of the thyroid), which can cause temporary hyperthyroidism because the inflamed thyroid releases its thyroxine stores into the bloodstream. Thyroiditis may happen due to an autoimmune problem, following pregnancy or after a viral infection. Thyroiditis is sometimes painful.
Hypothyroidism
Hypothyroidism is when you have an underactive thyroid. Symptoms usually develop gradually, sometimes over several years, and can include:
- weight gain;
- tiredness;
- feeling cold all the time, or sensitivity to the cold;
- constipation;
- dry skin;
- ‘puffy’ face;
- hair loss or thinning hair;
- hoarse voice;
- memory problems;
- feeling depressed;
- joint and muscle pain and/or stiffness;
- muscle weakness; and
- slow heartbeat (pulse).
Women with hypothyroidism may notice irregular or heavy periods.
Causes of hypothyroidism
Hashimoto thyroiditis (also called Hashimoto’s disease), an autoimmune condition, is the most common cause of hypothyroidism.
Damage to the thyroid from radiation treatment used to treat head or neck cancers or certain medicines (e.g. lithium, amiodarone, interferon alfa) can also cause hypothyroidism. And sometimes treatment for an overactive thyroid can unfortunately end up causing hypothyroidism.
Who gets thyroid problems?
Both underactive and overactive thyroid conditions are more common in women than men.
Hypothyroidism is more common in those older than 55 years of age.
If you have a family history of thyroid problems or have an autoimmune disease you are also at increased risk.
Complications
Untreated thyroid disorders can lead to other problems, such as heart disease, high cholesterol, high blood pressure and osteoporosis.
Diagnosis and tests
If you have noticed any swelling in the neck, or have noticed symptoms of an overactive or underactive thyroid, talk to your doctor. If your GP (general practitioner) suspects you have a thyroid problem, they will ask about your symptoms and do a physical examination, including examining your neck.
Both hyperthyroidism and hypothyroidism can be associated with generalised swelling of the thyroid, known as goitre. Thyroid nodules (non-cancerous lumps) and thyroid cancer may show up as firm, usually painless, lumps in the thyroid.
Simple blood tests can be done to assess your thyroid function and help work out the cause of your thyroid problem. Scans of your thyroid gland may sometimes also be needed to diagnose thyroid disease.
Your doctor may refer you to an endocrinologist (doctor who specialises in treating hormonal conditions such as thyroid disease) or a thyroid surgeon for further tests and treatment.
Thyroid function tests
Blood tests can be done to measure the levels of the different thyroid hormones – thyroid stimulating hormone (TSH), free T4 (thyroxine) and free T3 (triiodothyronine). (‘Free’ T3 and T4 measurements refer to the very small proportion of these hormones that circulate in the bloodstream unbound to proteins. By measuring the free hormones, the results are not affected by changes in the levels of thyroid hormone-binding proteins.)
Thyroid stimulating hormone (TSH) is the best initial test of thyroid function. If the TSH is abnormal, free T4 is then usually measured. Free T3 levels may also be measured if TSH is abnormal but free T4 is normal, or if free T4 is high.
People with thyroid function tests showing an abnormal TSH but normal free T4 and T3 levels may have what’s called subclinical (or mild) hypothyroidism or hyperthyroidism. These people often do not have any obvious symptoms. Subclinical hypothyroidism is more common than overt hypothyroidism.
| Typical thyroid function test results for thyroid disorders | |||
|---|---|---|---|
| TSH result | Free T4 result | Free T3 result | |
| Normal thyroid function | Normal range* is 0.45-4.5 mIU/L | Normal range* is 12-30 pmol/L | Normal range* is 2-7 pmol/L |
| Hyperthyroidism | Low | High | High |
| Sub-clinical, or mild, hyperthyroidism | Low | Normal | Normal |
| Hypothyroidism (primary) | High | Low | Low |
| Hypothyroidism (secondary or tertiary) | Low/normal | Low | Low |
| Sub-clinical, or mild hypothyroidism | High | Normal | Normal |
| *Note that different laboratories may have slightly different reference ranges for normal, so always follow the advice of your doctor. | |||
Thyroid antibody tests
Blood tests for thyroid antibodies can help work out the cause of your thyroid problem. The presence of TSH-receptor antibodies (TRAb) indicates Grave’s disease. Thyroid peroxidase antibodies (TPOAb) can be raised in people with Grave’s disease or Hashimoto thyroiditis, as well as other autoimmune thyroid problems.
Thyroid scans
Thyroid nuclear medicine scans can help work out the cause of hyperthyroidism (overactive thyroid). Radionuclide thyroid scanning can show whether the whole thyroid or a nodule (or nodules) within the thyroid is overactive. You are injected with a small amount of radioactive substance and then scanned to look at the uptake of the ‘tracer’ by your thyroid. Scans can show the structure and the function of your thyroid gland.
An ultrasound scan may be needed if there is swelling of the thyroid or a lump. Ultrasound scans can show whether a lump is cystic (fluid-filled) or solid.
Brain scans may be recommended if problems with the pituitary gland are thought to be causing the thyroid dysfunction.
Treating hyperthyroidism
Treatment for hyperthyroidism depends on the cause. Other factors, such as your age and general health, and the severity of your hyperthyroidism will also help determine the best treatment for you.
Grave’s disease is usually treated with medicines which suppress the formation of T3 and T4. Carbimazole (brand name Neo-Mercazole) is the antithyroid medicine usually prescribed, but propylthiouracil (PTU Tablets) may be used in some circumstances. Radioactive iodine (which shrinks the thyroid gland) or surgery (removing all or most of the gland) are other treatment options that may also be recommended.
Toxic multinodular goitre and toxic adenomas are usually treated with surgery or radioactive iodine. Antithyroid medicines may also be recommended.
Thyroiditis often doesn’t need specific treatment, but beta-blocker medicines and pain relievers may be given to treat symptoms.
Sub-clinical hyperthyroidism often gets better without treatment but follow-up thyroid function testing is recommended.
Many people who are treated for hyperthyroidism develop hypothyroidism, either straight away or over time. Long-term monitoring with thyroid function tests is recommended for all people with thyroid disorders.
Hypothyroidism treatments
Treatment for hypothyroidism involves taking thyroxine, usually levothyroxine tablets (brand names include Eltroxin, Eutroxsig and Oroxine). Thyroxine replacement aims to return your thyroid hormone levels to normal as well as relieve symptoms. It can take a few months to get the dose just right for you – you’ll need to have thyroid function tests every 4-8 weeks when you start treatment to guide the dose.
Most people with hypothyroidism will need lifelong treatment with levothyroxine and ongoing monitoring of their thyroid function.
Treatment of subclinical hypothyroidism will depend on your symptoms (or lack of symptoms), TSH level, age and general health. Thyroxine tablets may be recommended for some people, while for others ongoing monitoring of thyroid function may be all that is needed.
Some studies have found that taking selenium supplements improves quality of life in certain people with Hashimoto’s thyroiditis.
Support for people with thyroid conditions
Support is available for people with thyroid conditions. Ask your doctor or search online for a thyroid support group that meets your needs, whether it be a group that meets in person or an online community. Support groups provide information and understanding of thyroid problems and ways to help recovery.

