There is no single, simple test to detect prostate cancer. Two commonly used tests are the PSA (prostate specific antigen) blood test and the digital rectal examination. However, these tests, used separately or in combination, only show changes in the prostate. They do not diagnose cancer. If either test shows an abnormality, your GP will refer you to a urologist for further evaluation.
There are Australian guidelines to help health professionals decide on the best approach to PSA testing and other early tests for prostate cancer.
Prostate specific antigen (PSA) blood test
Prostate specific antigen (PSA) is a protein made by both normal prostate cells and cancerous prostate cells. PSA levels are measured using a blood test. The PSA test does not specifically test for cancer.
A PSA reading that is above the typical range for your age (e.g. above 3 nanograms per millilitre for men aged 50−59) or that is rising rapidly may indicate the possibility of prostate cancer. However, only one in three men with a higher PSA level has cancer. The amount of PSA in the blood can be raised even when a man does not have cancer. Other factors can increase PSA levels, including:
- benign prostate hyperplasia
- recent sexual activity
- an infection in the prostate
- or a recent digital rectal examination.
In addition, some men with prostate cancer have normal PSA levels.
Because PSA levels can vary in an individual from day to day, your doctor will often use results from more than one blood test, over time, to help determine your risk of prostate cancer. Other blood tests your doctor may suggest include:
Free PSA test
Measures the PSA molecules in your blood that are not attached to other blood proteins (free PSA). This test may be suggested if your PSA score is moderately raised and your doctor is not sure whether you need a biopsy. A low level of free PSA compared to the total PSA may indicate prostate cancer.
Prostate health index (PHI)
Measures three different forms of the PSA protein. This test is not widely used in Australia.
Digital rectal examination (DRE)
To do a digital rectal examination (DRE), the specialist inserts a gloved finger into your rectum to feel the back of the prostate. The DRE may be uncomfortable, but is rarely painful. If the specialist feels a hardened area or an odd shape, further tests may be done. Abnormalities do not always indicate prostate cancer. On the other hand, a normal DRE does not rule out prostate cancer, as the examination is unlikely to pick up a small cancer or one the finger can’t reach.
Digital rectal examination is no longer recommended as a routine test for men who do not have symptoms of prostate cancer. However, not all prostate cancers produce high levels of PSA, so the specialist may use a DRE to check the prostate before doing a biopsy.
MRI scan
An MRI (magnetic resonance imaging) scan uses a powerful magnet and radio waves to build up detailed pictures of the inside of the body. The main type of MRI used for men suspected of having prostate cancer is the mpMRI (multi-parametric magnetic resonance imaging) scan. This combines the results of three MRI scans to provide a clearer image.
An MRI can show abnormal areas of the prostate. Your doctor may suggest this scan to help work out if a biopsy is needed and which areas to biopsy. An MRI can also help show whether the cancer has spread from the prostate to nearby areas.
Before an MRI scan, a dye may be injected into a vein to make the pictures clearer. You will lie on an examination table that slides into a large metal cylinder that is open at both ends. The scan is painless but can be noisy and may take 30–40 minutes. Some people feel claustrophobic in the cylinder. Talk to your doctor or nurse before the scan if you feel anxious in confined spaces. Also let them know if you have a pacemaker or any other metallic object in your body. The magnet can interfere with some pacemakers, but newer pacemakers are MRI-compatible.
The dye used in an MRI scan or CT scan can cause allergies. If you have had a reaction to dyes during a previous scan, tell your medical team beforehand. You should also let them know if you are diabetic or have kidney disease.
At the time of publication, Medicare does not provide a rebate for MRI and PET scans for prostate cancer. The mpMRI and PET scans are not available at all hospitals. Ask your doctor for more information about availability and costs.
Biopsy
If the PSA test or DRE show an abnormality, a biopsy is often the next step. In some cases, your doctor will suggest an MRI scan before doing a biopsy.
During a biopsy, small amounts of tissue are taken from different parts of the prostate using a special needle. The samples are sent to a laboratory, where a specialist doctor called a pathologist examines the tissue for cancer cells.
A biopsy is usually done with the help of a transrectal ultrasound (TRUS). A small probe is inserted into the rectum and sends out soundwaves. A computer creates an image based on the echoes produced when the soundwaves meet the prostate. Using the TRUS image as a guide, the doctor inserts a thin, hollow needle into the prostate. The needle is inserted either through the rectum (transrectal) or through the skin between the anus and the scrotum (transperineal).
A biopsy can be uncomfortable and for a few days there may be a small amount of blood in your urine, semen or bowel motions. It usually takes about a week for the biopsy results to come back.
Further tests
If the biopsy shows prostate cancer, other tests may be done to work out whether it has spread. You may also have regular blood tests to check PSA, prostate cancer activity and general health.
Bone scan
This scan can show whether the prostate cancer has spread to your bones. A tiny amount of radioactive substance will be injected into a vein. You will need to wait for 1–2 hours while the substance moves through your bloodstream to your bones. Your whole body will then be scanned with a machine that detects radioactivity. A larger amount of radioactivity will show up in any areas of bone with cancer cells. The scan is painless, and the radioactive substance disappears from your body in a few hours.
CT scan
A CT (computerised tomography) scan uses x-ray beams to create detailed pictures of the inside of the body. A CT scan of the abdomen can show whether cancer has spread to lymph nodes in that area. A dye is injected into a vein to help make the scan pictures clearer. You will lie still on a table that moves slowly through the CT scanner, which is large and round like a doughnut. The scan itself takes a few minutes and is painless, but the preparation takes 10–30 minutes.
PET scan
A PET (positron emission tomography) scan is a sensitive scan that may help detect cancer that has come back or spread. It involves the injection of a small amount of a radioactive solution. Cancer cells take up more of this solution and show up brighter on the scan. For prostate cancer, the solution is usually one that detects prostate specific membrane antigen (PSMA).
Staging and grading
Your specialist will assign a stage and grade to your cancer, which will help you and your health care team decide which treatment or management option is best for you.
Staging
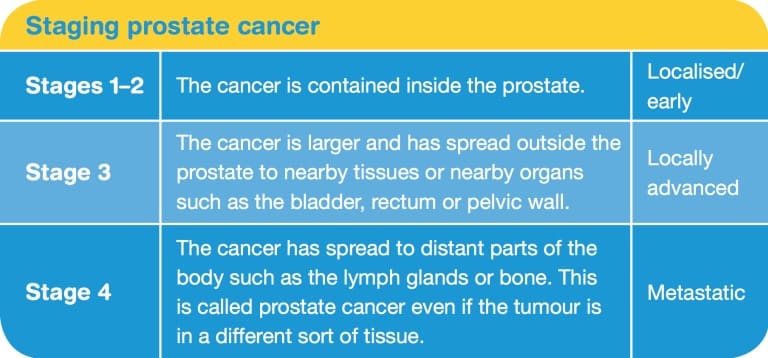
Staging is the process of working out how large the cancer is and whether it has spread to other parts of the body. Prostate cancer is staged using the TNM system. The specialist assigns numbers for the size of the tumour (T), whether the cancer has spread to nearby lymph nodes (N), and whether the cancer has spread to the bones or other organs, i.e. whether it has metastasised (M). The lower the number, the less advanced the cancer.
The TNM scores are combined to work out the overall stage of the cancer, from stage 1 to stage 4 (see below). Stages 3 and 4 are both considered advanced prostate cancer.
Grading
Grading describes how likely the cancer is to spread. A doctor called a pathologist works this out using a microscope to look
at cells from a biopsy. Low-grade cancer cells tend to grow slowly, while high-grade cancer cells look abnormal and grow faster.
For many years, the Gleason scoring system has been used for grading the tissue taken during a biopsy. All men with prostate cancer will have a Gleason score between 6 and 10. A new system has been introduced to replace the Gleason system. Known as the Grade Group system, this grades prostate cancer from 1 (least aggressive) to 5 (most aggressive).

Risk of progression
For men diagnosed with localised prostate cancer, the specialist will assign a level of low, intermediate or high risk to indicate how likely the cancer is to grow and spread. This is known as the risk of progression. Your doctor will work out this risk by considering the stage and grade, as well as your PSA level before the biopsy and your overall health, age and wishes. The risk category helps guide management and treatment.
Prognosis
Prognosis means the expected outcome of a disease. In general, the prognosis is better when prostate cancer is diagnosed while it is localised and at a lower grade.
You may wish to discuss your prognosis with your specialist. However, it is not possible for anyone to predict the exact course of the cancer. Test results, whether the cancer has spread (its stage), how quickly it might grow (its grade), and factors such as your age, level of fitness, and medical and family history are all important in assessing your prognosis.
Prostate cancer often grows slowly and even the more aggressive cases of prostate cancer tend to grow more slowly than other types of cancer. Compared with other cancers, prostate cancer has one of the highest five-year survival rates. For many men, prostate cancer grows so slowly that it never needs treatment. They live with prostate cancer for many years without any symptoms and without it spreading.
Key points
- Your doctor may test the level of a protein called prostate specific antigen (PSA) in your blood. Some men with prostate cancer may have a higher PSA level, while a small number do not.
- Your doctor may do a digital rectal examination (DRE) by inserting a gloved finger into your rectum to feel the prostate.
- An mpMRI scan may help work out if you need a biopsy.
- If tests show abnormalities, some tissue may be removed from the prostate for examination in a laboratory. This is called a biopsy.
- You may have other tests to check the extent of the prostate cancer, including a bone scan or CT scan.
- A specialist doctor such as a urologist will assign a stage to the cancer. This describes if and how far the cancer has spread. The TNM (tumour– nodes–metastasis) system is used to give an overall stage of 1–4. The cancer may also be described as localised, locally advanced, advanced or metastatic.
- Test results will provide information about the grade and size of the cancer. The grade tells how fast the cancer may grow. Your specialist will describe the grade using the Gleason or Grade Group score.
- Localised prostate cancer is also categorised as having a low, intermediate or high risk of progression. This helps the specialist work out the best approach to treatment.
- Your specialist may talk to you about your prognosis, which is the expected outcome of the disease.

