Making treatment decisions
Sometimes it is difficult to decide on the type of treatment to have. You may feel that everything is happening too fast, or you might be anxious to get started. Check with your specialist how soon treatment should begin – often it won’t affect the success of the treatment to wait a while. Ask them to explain the options, and take as much time as you can before making a decision.
Know your options
Understanding the disease, the available treatments, possible side effects and any extra costs can help you weigh up the options and make a well-informed decision. Check if the specialist is part of a multidisciplinary team and if the treatment centre is the most appropriate one for you – you may be able to have treatment closer to home, or it might be worth travelling to a centre that specialises in a particular treatment.
Record the details
When your doctor first tells you that you have cancer, you may not remember everything you are told. Taking notes or recording the discussion can help. It is a good idea to have a family member or friend go with you to appointments to join in the discussion, write notes or simply listen.
Ask questions
If you are confused or want to check anything, it is important to ask your specialist questions. Try to prepare a list before appointments. If you have a lot of questions, you could talk to a cancer care coordinator or nurse.
Consider a second opinion
You may want to get a second opinion from another specialist to confirm or clarify your specialist’s recommendations or reassure you that you have explored all of your options. Specialists are used to people doing this. Your GP or specialist can refer you to another specialist and send your initial results to that person. You can get a second opinion even if you have started treatment or still want to be treated by your first doctor. You might decide you would prefer to be treated by the second specialist.
It’s your decision
Adults have the right to accept or refuse any treatment that they are offered. For example, some people with advanced cancer choose treatment that has significant side effects even if it gives only a small benefit for a short period of time. Others decide to focus their treatment on quality of life. You may want to discuss your decision with the treatment team, GP, family and friends.
Should I join a clinical trial?
Your doctor or nurse may suggest you take part in a clinical trial. Doctors run clinical trials to test new or modified treatments and ways of diagnosing disease to see if they are better than current methods. For example, if you join a randomised trial for a new treatment, you will be chosen at random to receive either the best existing treatment or the modified new treatment. Over the years, trials have improved treatments and led to better outcomes for people diagnosed with cancer.
You may find it helpful to talk to your specialist, clinical trials nurse or GP, or to get a second opinion. If you decide to take part in a clinical trial, you can withdraw at any time. For more information, visit australiancancertrials.gov.au.
Treatment for early bowel cancer
Treatment for early and locally advanced bowel cancer will depend on the type of bowel cancer you have. This is because colon cancer and rectal cancer are treated differently.
Your medical team will recommend treatment based on what will give you the best outcome, where the cancer is in the bowel, whether and how the cancer has spread, your general health, and your preferences.
The treatment options you are offered will depend on the guidelines for best practice in treating bowel cancer. For some people, the best option may be to join a clinical trial (see above).
Treatment options by type of bowel cancer
Colon cancer
- Surgery is the main treatment for early and locally advanced colon cancer.
- If the cancer has spread to the lymph nodes, you may have chemotherapy after surgery. This is called adjuvant chemotherapy.
- Radiation therapy is not used for early colon cancer.
Rectal cancer
- Surgery is the main treatment for early rectal cancer.
- If the cancer has spread beyond the rectal wall and/or into nearby lymph nodes (locally advanced cancer), before the surgery you will have either radiation therapy or chemotherapy combined with radiation therapy (chemoradiation). After the surgery you may have chemotherapy.
Preparing for treatment
Managing anaemia
Many people with bowel cancer have anaemia or low iron levels. You may be given iron as tablets or intravenously to improve your iron levels and blood count before treatment begins.
Improve diet and nutrition
People with bowel cancer often lose a lot of weight and may become malnourished. A dietitian can provide advice on ways to reduce the weight loss through changes to your diet or liquid nutritional supplements. This will help improve your strength and lead to better treatment outcomes.
Surgery
The type of surgery you have will depend on the location of the cancer in the bowel and your preferences. The aim of surgery is to remove as much of the cancer as possible and nearby lymph nodes.
How the surgery is done
There are two ways to perform surgery for bowel cancer. Each method has advantages in particular situations – your doctor will advise which method is most suitable for you.
Keyhole surgery
Also called minimally invasive or laparoscopic surgery, this method involves several small cuts (incisions) in the abdomen. A thin tube (laparoscope) is passed through one of the cuts. The laparoscope has a light and camera. Long, thin instruments are inserted through other small cuts to remove the section of bowel with the cancer. Keyhole surgery usually means less pain and scarring, a shorter hospital stay and faster recovery.
Open surgery
This involves one long cut (incision) down the middle of your abdomen. Open surgery usually means a larger wound and slower recovery, and it requires a longer hospital stay. Open surgery is a well-established technique and widely available.
Surgery for cancer in the colon
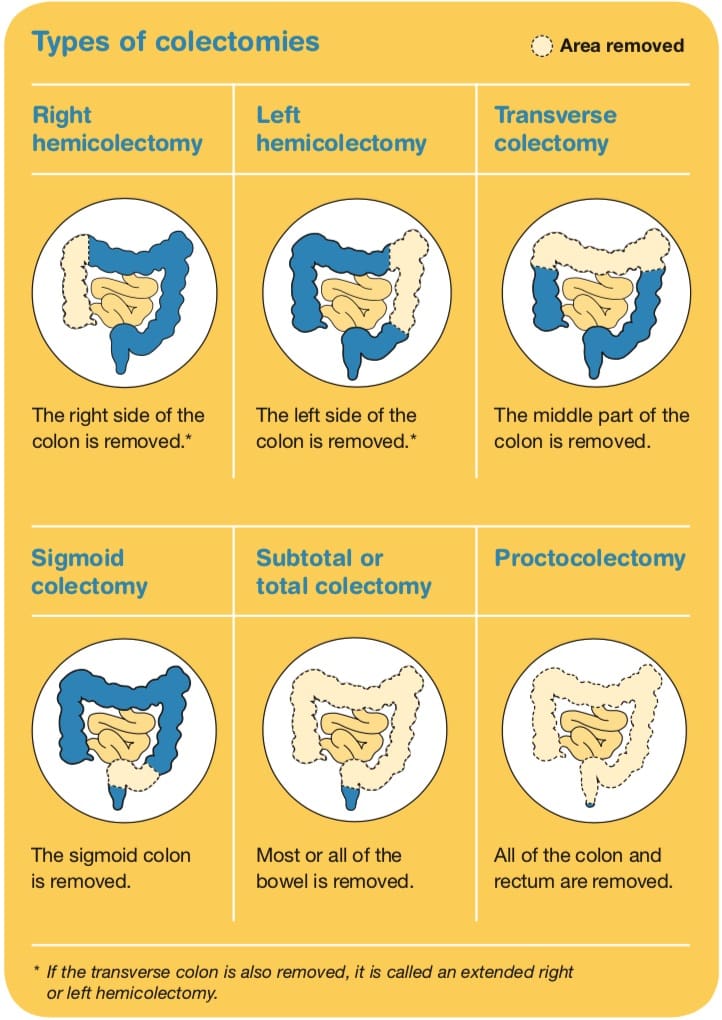
The most common type of surgery for colon cancer is a colectomy.
It may be done as open surgery or keyhole surgery (see above). There are different types of colectomies depending on which part of the colon is removed (see below). Lymph nodes near the colon and some normal bowel around the cancer will also be removed.
The surgeon usually cuts the bowel on either side of the cancer (with a small border of healthy tissue called the margin) and then joins the two ends of the bowel back together. This join is called an anastomosis.
Sometimes one end of the bowel is brought through an opening made in your abdomen and stitched onto the skin. This procedure is called a colostomy (if made from the large bowel) or ileostomy (if made from the small bowel). The opening – called a stoma – allows faeces to be removed from the body and collected in a bag.
The stoma is usually temporary, and the operation is reversed later. In some cases, the stoma is permanent. Advances in surgical techniques have led to fewer people needing a permanent stoma. See below for further information about stomas.
After surgery, you will have a scar. Most people who have open surgery have a scar from above their navel to their pubic area.
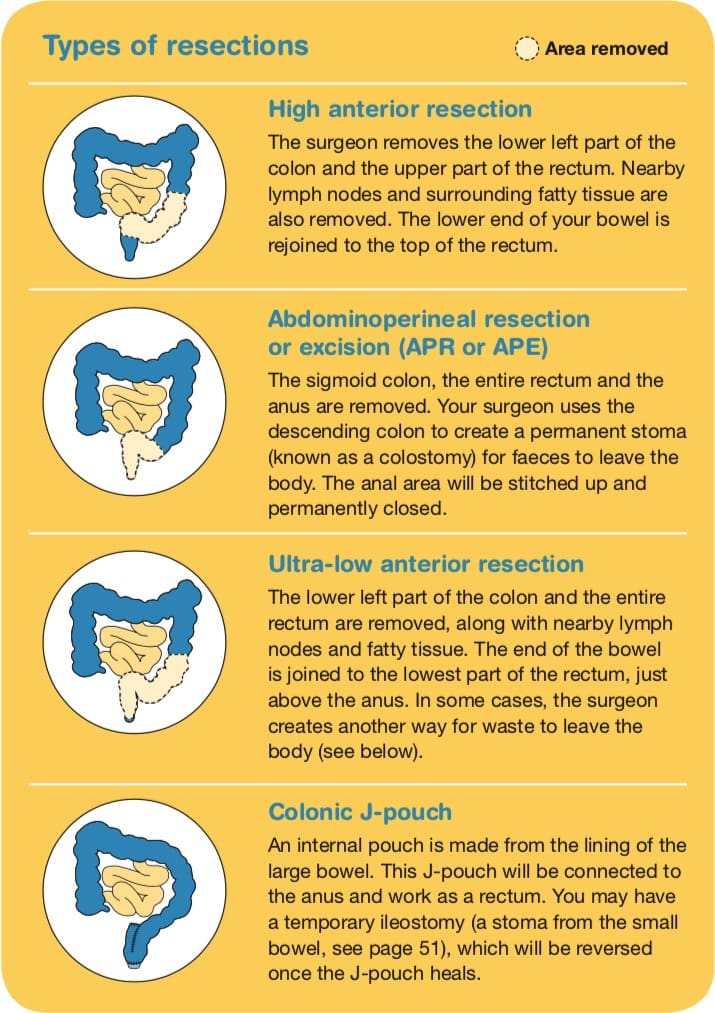
Surgery for cancer in the rectum
There are different types of operations for cancer in the rectum (see above). The type of operation you have depends on where the cancer is located, whether the bowel can be rejoined, and where in the rectum the join can be made.
The surgery may be performed using an open or keyhole approach (see above). You may have an anterior resection or abdominoperineal resection (also known as an abdominoperineal excision).
Anterior resection
This is the most common operation. It may include creating a temporary stoma, which will be reversed later.
Abdominoperineal resection
This procedure may be recommended if the cancer is near the anal sphincter muscles or if it is too low to be removed without causing incontinence (accidental loss of faeces). After an abdominoperineal resection you will need a permanent stoma (colostomy). Speak to your surgeon about any concerns you may have.
Other types of surgery
Local excision
People who have very early stage rectal cancer or are not fit for a major operation may have a local excision. The surgeon inserts an instrument into the anus to remove the cancer from the lining of the rectum, along with a margin of healthy tissue, without cutting into the abdomen. Methods include transanal excision (TAE), transanal endoscopic microsurgery (TEMS) and transanal minimally invasive surgery (TAMIS).
If there are two cancers
In a small number of people, two separate cancers may be found in the large bowel at the same time. The cancers may be discovered through diagnostic tests or during surgery. In this case, there are several options for surgery:
- remove two sections of the bowel
- remove one larger section of the bowel, which includes both areas with cancer
- remove the entire colon and rectum (proctocolectomy) to prevent any chance of another cancer forming.
The type of surgery your doctor recommends depends on several factors including your age, the location of the tumours in the bowel, genetic and other risk factors, and your preferences.
Surgery for a blocked bowel (bowel obstruction)
Sometimes as the bowel cancer grows it completely blocks the bowel. This is called bowel obstruction. Waste matter cannot pass through the blocked bowel easily, and may cause:
- bloating and abdominal pain
- constipation
- nausea and vomiting.
Sometimes the obstruction is found and cleared during the surgery to remove the cancer. In other cases, the bowel obstruction will mean you have to have emergency surgery to clear the blockage.
It may be possible to rejoin the bowel during the surgery, but some people may need a stoma (see pages 50–55). Sometimes a stoma is made “upstream” from the obstruction to relieve the blockage and to allow time for staging scans of the cancer or chemoradiation before surgery, to make sure the cancer is removed completely.
Not everyone with a blockage will want to have surgery or be fit enough to have it. To help keep the bowel open so that stools can pass through again, your surgeon may be able to insert a small hollow tube (stent) inside the colon. A stent may also help manage the blockage until you are well enough to have an operation. Your surgeon will use a colonoscope to find the blockage and place the stent.
If you are unable to have surgery or a stent, you may be given medicine to help control the symptoms of a bowel obstruction.
Risks of bowel surgery
Your surgeon will talk to you about the risks and complications of bowel surgery. As with any major operation, bowel surgery has risks. Complications may include infection, bleeding, blood clots, damage to nearby organs, or leaking from the joins between the removed parts of the bowel. You will be carefully monitored for any side effects afterwards.
It may be possible to rejoin the bowel during the surgery, but some people may need a stoma (see below). Sometimes a stoma is made “upstream” from the obstruction to relieve the blockage.
Most hospitals in Australia have programs to reduce the stress of surgery and improve your recovery. These are called enhanced recovery after surgery (ERAS) or fast track surgical (FTS) programs, and they encourage you to play an active part in your care through pre-admission counselling, and education about pain control, diet and exercise so you know what to expect each day after the surgery.
What to expect after surgery
This is a general overview of what to expect. The process varies from hospital to hospital, and everyone will respond to surgery differently.
Recovery time
- Your recovery time after the operation will depend on your age, the type of surgery you had and your general health.
- You will probably be in hospital for 4–7 days, but it can take 2–3 months to fully recover.
- You will have to wear compression stockings while you are in hospital to help the blood in your legs to circulate.
- You will also be given a daily injection of a blood thinner to reduce the risk of developing blood clots.
- Some people also wear a special cuff that applies intermittent pressure to the legs.
- Some people may have to wear the stockings and have the injections for a couple of weeks after the surgery.
Pain relief
- You will have some pain and discomfort for several days after surgery, but you will be given pain-relieving medicines to manage this.
- Pain relief may be given in various ways:
- by an injection near your spinal column (epidural or spinal anaesthetic)
- through a drip which you can control with a button (PCA – patient controlled analgesia)
- as pills or tablets
- through little tubes giving local anaesthetic near your wound (TAP block catheters).
- Let your doctor or nurse know if you are in pain so they can adjust the medicines to make you as comfortable as possible. Do not wait until the pain is severe.
Drips and tubes
- You will be given fluids through a drip (also called an intravenous or IV infusion) until you can start eating and drinking again. You may need a drip for a few days.
- You may also have other tubes – from your bladder to drain urine (catheter) or from your abdomen to drain fluid from around the surgical area.
- In most centres, you will be given water to drink a few hours after the surgery and you will usually start on solid foods the day after the surgery (or even on the day of the surgery if you feel well). You may also be given nutritional supplements to drink.
- In some centres, you will not have anything to eat or drink for several days after the surgery.
Activity/exercise
- Your health care team will encourage you to walk the day after the surgery.
- You will need to avoid heavy lifting (more than 3–4 kg) for about 4–6 weeks.
- A physiotherapist will teach you breathing or coughing exercises to help keep your lungs clear. This will reduce the risk of getting a chest infection.
- Gentle exercise has been shown to help people manage some of the common side effects of treatment and speed up a return to usual activities.
Side effects of bowel surgery
Changes in bowel and sexual function
Many people find that their bowel and bladder functions change. These usually improve within a few months but, for some people, it can take longer. Erection problems can also be an issue for some men after rectal cancer surgery.
Changes to your diet – See also Bowel cancer: managing bowel and dietary changes
Fatigue – It is normal to feel tired after surgery. Although it’s a good idea to stay active and do gentle exercise as recommended by your doctor, you may find that you tire easily and need to rest during the day. Take breaks if you feel tired, and follow your doctor’s advice about restrictions, such as avoiding heavy lifting. You might have to remind your family and friends that it may take several months to recover from surgery.
Temporary or permanent stoma – See Having a stoma
Radiation therapy
Also known as radiotherapy, this treatment uses a controlled dose of radiation, such as focused x-ray beams, to kill or damage cancer cells. The radiation is targeted to the specific area of the cancer, and treatment is carefully planned to do as little harm as possible to your normal body tissue near the cancer. Radiation therapy is often combined with chemotherapy (chemoradiation). This is because chemotherapy makes cancer cells more sensitive to radiation.
Radiation therapy is not generally used to treat locally advanced colon cancer. Commonly, a short course of radiation therapy or a longer course of chemoradiation is used to shrink the tumour before surgery for locally advanced rectal cancer. The aim of this treatment is to make the cancer as small as possible before it is removed. This means it will be easier for the surgeon to completely remove the tumour and reduces the risk of the cancer coming back.
Occasionally, if the rectal cancer is found to be more advanced than originally thought, radiation therapy may be used after surgery to destroy any remaining cancer cells.
External beam radiation therapy is the most common type of radiation therapy for rectal cancer. Newer techniques deliver the dose to the affected area without damaging surrounding tissue. These improvements have reduced the side effects from radiation therapy.
During treatment, you will lie on a treatment table under a machine called a linear accelerator. Each treatment takes only a few minutes, but a session may last 10–20 minutes because of the time it takes to set up the machine.
There will be a break between radiation therapy and surgery to allow the treatment to have its full effect. If radiation therapy is given with chemotherapy, you will have it once a day for 5–6 weeks, then there will be a gap of 6–12 weeks before surgery. If radiation therapy is given by itself, you will have a shorter course, usually for five days, then a shorter gap before surgery.
Side effects of radiation therapy
The side effects of radiation therapy vary. Most are temporary and disappear a few weeks or months after treatment. Radiation therapy for rectal cancer is usually given over the pelvic area, which can irritate the bowel and bladder.
Common side effects include feeling tired, needing to pass urine more often and burning when you pass urine (cystitis), redness and soreness in the treatment area, diarrhoea, constipation or faecal urgency and incontinence. Radiation therapy can cause the skin or internal tissue to become less stretchy and harden (fibrosis). It can also affect fertility and sexual function, see below.
People react to radiation therapy differently, so some people may have few side effects, while others have more. Your treatment team will give you advice about possible side effects and how to manage them.
Radiation proctitis
Radiation to the pelvic area can damage the lining of the rectum, causing inflammation and swelling (known as radiation proctitis). This can cause a range of symptoms including diarrhoea, the need to empty the bowels urgently and loss of control over the bowels (faecal incontinence). When treating rectal cancer, these side effects may appear shortly after radiation therapy, but are generally not a problem long term because the rectum is removed during surgery. Your treatment team will talk to you about your risk of developing radiation proctitis. .
Effects on fertility and sexual function
Radiation therapy to the pelvis and rectum can affect your ability to have children (fertility) and sexual function.
For men
- Radiation therapy can damage sperm or reduce sperm production. This may be temporary or permanent.
- Most doctors suggest that men use contraception and don’t have unprotected sex during and for one month after radiation therapy.
- You will be able to store sperm at a hospital or fertility clinic before treatment starts. Talk to your doctor about this.
- Because radiation therapy can damage blood vessels and nerves that produce erections, some men may have erection problems. Your doctor may prescribe medicine or refer you to a specialist clinic to manage this problem.
For women
- Radiation therapy can lead to the vagina becoming shorter and narrower, making sexual intercourse painful. Your doctor may suggest you use a vaginal dilator after radiation therapy is finished to help gradually widen the entrance and prevent the side walls sticking together. Using dilators can be challenging. Your doctor or a physiotherapist can provide practical advice on using a dilator.
- Talk to your doctor about creams and moisturisers to help with vaginal discomfort and dryness.
- In some cases, radiation therapy can stop the ovaries producing female hormones. This can cause menopause and infertility.
- Menopause can be managed by hormone replacement therapy, which can be taken if you’ve had rectal cancer. After menopause you will not be able to conceive a child.
- Share your feelings about any fertility issues with your partner, a counsellor or a fertility specialist.
Chemotherapy
Chemotherapy uses drugs to kill or slow the growth of cancer cells while doing the least possible damage to healthy cells. If the cancer has spread outside the bowel to lymph nodes or to other organs, chemotherapy may be recommended:
Before surgery (neoadjuvant) – Some people with locally advanced rectal cancer have chemotherapy before surgery to shrink the tumour and make it easier to remove. You are likely to have chemotherapy together with radiation therapy (chemoradiation).
After surgery (adjuvant) – Chemotherapy may be used after surgery for either colon or rectal cancer to get rid of any remaining cancer cells and reduce the chance of the cancer coming back. If your doctor recommends chemotherapy, you will probably start as soon as your wounds have healed and you’ve recovered your strength, usually within eight weeks.
On its own – If the cancer has spread to other organs, such as the liver or lungs, chemotherapy may be used either to shrink the tumours or to reduce symptoms and make you more comfortable.
You may have chemotherapy through a liquid drip into a vein (intravenously) or as tablets. It may also be given through a thin plastic tube called a central venous access device. Some people have chemotherapy at home through a portable bottle called an infusor pump. You will probably have chemotherapy as a course of several sessions (cycles) over 4–6 months. Your medical oncologist will explain your treatment schedule.
Side effects of chemotherapy
People react to chemotherapy differently – some people have few side effects, while others have many. The side effects depend on the drugs used and the dose. Your medical oncologist or nurse will discuss the likely side effects with you, including how they can be prevented or controlled with medicine. It is uncommon to need a break or change in your treatment.
Common side effects include tiredness; feeling sick (nausea and vomiting); diarrhoea; mouth sores and ulcers; changes in appetite, taste and smell; sore hands and feet; and hair loss or thinning. You may also be more likely to catch infections.
Pins and needles, numbness, redness or swelling in the fingers and toes are more common if using the chemotherapy drug called oxaliplatin. Skin peeling and increased sensitivity to sunlight are more common if using the chemotherapy drug called fluorouracil (or 5-FU).
Keep a record of the doses and names of your chemotherapy drugs handy. This will save time if you become ill and need to visit the emergency department.
During chemotherapy, you will have a higher risk of getting an infection or bleeding. If you have a temperature over 38°C, contact your doctor or go to the emergency department. Tell your doctor if you feel more tired than usual, or if you bruise or bleed easily.
Key points about treating early bowel cancer
Treatments for early colon cancer
- The main treatment is surgery to remove part or all of the colon (colectomy).
- There are different types of colectomies depending on where the cancer is located.
- If cancer has spread from the colon to nearby lymph nodes, you may have chemotherapy after surgery.
Treatments for early rectal cancer
- The main treatment is surgery to remove all or part of the rectum (resection).
- There are different types of resections depending on where the cancer is located.
- If cancer has spread from the rectum into nearby tissue or lymph nodes, you will usually have radiation therapy or chemoradiation before the surgery.
- A local excision to remove the cancer may occasionally be used for very early stage rectal cancer.
How surgery is done
- Surgery for bowel cancer may be done as keyhole surgery (several smaller cuts) using a tiny surgical instrument with a camera and light, or open surgery (one large cut).
- During bowel surgery, the surgeon cuts the bowel on either side of the cancer and joins the two ends back together.
- If it is not possible to join the bowel back together or if the bowel needs time to heal, a diversion is created for faeces to come through a hole (stoma) in the abdominal wall.
Treatment for advanced bowel cancer
When bowel cancer has spread to the liver, lung or lining of the abdomen and pelvis (omentum and peritoneum), this is known as advanced or metastatic (stage 4) bowel cancer. To control the cancer, slow its growth and manage symptoms such as pain, you may have a combination of chemotherapy, targeted therapy, radiation therapy and surgery.
Systemic treatment
Advanced bowel cancer is commonly treated with drugs that reach cancer cells throughout the body. This is called systemic treatment, and includes chemotherapy (see above) and targeted therapy.
Targeted therapy drugs work differently from chemotherapy drugs. While chemotherapy drugs affect all rapidly dividing cells and kill cancerous cells, targeted therapy drugs affect specific molecules within cells to block cell growth.
Monoclonal antibodies are the main type of targeted therapy drug used in Australia for advanced bowel cancer. They include:
Bevacizumab
This drug stops the cancer developing new blood cells and growing. It is given as a drip into a vein (intravenous infusion) every two to three weeks, with chemotherapy.
Cetuximab and panitumumab
These drugs target specific features of cancer cells known as epidermal growth factor receptors (EGFR). They only work for people who have a normal RAS gene (known as RAS wild-type). The tumour will be tested for changes (mutations) in these genes before you are offered these drugs (see above under Molecular testing). These drugs are usually given as a drip into a vein (intravenous infusion). They may be given with chemotherapy or on their own after other chemotherapy drugs have stopped working.
Other types of targeted therapy drugs may be available on a clinical trial (see above). Talk with your doctor about the latest developments and whether you are a suitable candidate.
Scans and blood tests will be used to monitor your response to systemic treatments. If results show that the cancer is shrinking or is under control, chemotherapy and/or targeted therapy will continue. If the cancer is growing, that treatment will stop and alternative treatments will be discussed.
Side effects of targeted therapy
The side effects of targeted therapy vary depending on the drugs used. Common side effects of bevacizumab include high blood pressure, tiredness, bleeding and headaches. The most common side effects of cetuximab and panitumumab are skin problems (redness, swelling, an acne-like rash or dry, flaky skin), tiredness and diarrhoea.
Radiation therapy
Radiation therapy can also be used as a palliative treatment for both advanced colon and advanced rectal cancer. It can be used to stop bleeding and, if the cancer has spread to the bone or formed a mass in the pelvis, it can reduce pain. For further details, see above Radiation therapy.
Surgery
If the cancer has spread to other parts of the body, you may still be offered surgery. This can help remove some secondary cancers (e.g. in the liver or lungs) or relieve a bowel obstruction (see above).
You may have surgery to remove parts of the bowel along with all or part of other affected organs. This may be called an en-bloc resection or, if the cancer is in your pelvis, an exenteration.
If the cancer has spread to the lining of the abdomen (peritoneum), you may have surgery to remove as many tumours as possible. This is known as a peritonectomy or cytoreductive surgery. Sometimes, a heated chemotherapy solution is inserted into the abdomen during a peritonectomy. This is called hyperthermic intraperitoneal chemotherapy (HIPEC). Recent studies suggest that surgery alone may be as effective as surgery followed by HIPEC, and ongoing research continues to test the best approach to treatment.
The type of operation used for advanced bowel cancer will depend on your situation, so talk to your surgeon about what to expect. Your medical team will advise what kind of follow-up and treatment is recommended after surgery. Regular check-ups have been found to improve survival for people after surgery for bowel cancer, so you should have check-ups for several years.
Many treatments for advanced bowel cancer are best performed in a specialised centre. Call 13 11 20 for more information or to ask about assistance that may be available if you have to travel a long way.
Other treatments
If the cancer cannot be removed with surgery, but has only spread to a small number of places in a single area, your doctor may recommend another type of treatment to destroy or control the cancer. These treatments, including thermal ablation, selective internal radiation therapy (SIRT) and stereotactic body radiation therapy (SBRT), are only suitable for some people. They are best performed in a specialised centre or may be offered as part of a clinical trial.
Palliative treatment
Palliative treatment helps to improve people’s quality of life by managing the symptoms of cancer without trying to cure the disease. It is best thought of as supportive care.
Many people think that palliative treatment is for people at the end of their life, but it may help at any stage of advanced bowel cancer. It is about living for as long as possible in the most satisfying way you can.
Sometimes treatments such as surgery, chemotherapy, radiation therapy or targeted therapy are given palliatively. The aim is to help relieve symptoms such as pain or bleeding by shrinking or slowing the growth of the cancer.
Palliative treatment is one aspect of palliative care, in which a team of health professionals aim to meet your physical, emotional, practical, social and spiritual needs.
Key points about advanced bowel cancer
What it is
Advanced bowel cancer is cancer that has spread from the bowel to another part of the body or come back after the initial treatment.
Treatment goal
Treatment aims to control the cancer, slow down its spread and manage any symptoms.
The main treatment
Systemic treatments, including chemotherapy and targeted therapy, are used to control the cancer’s growth and stop it spreading.
Targeted therapy
Monoclonal antibodies are the main type of targeted therapy drug used for advanced bowel cancer. They include bevacizumab, cetuximab and panitumumab. The tumour may need to be tested to see if these drugs will be effective.
Other treatment options
Other options might include chemotherapy, radiation therapy, surgery, and palliative treatments. For some people, the best option may be to join a clinical trial.
Treatment side effects
All treatments can cause side effects, such as pain, tiredness, skin problems or diarrhoea. Talk to your doctor about how to manage any side effects.





